Drug Interaction Dose Calculator
Dose Adjustment Calculator
This tool calculates safe dose adjustments for digoxin and warfarin when adding amiodarone. Always consult your healthcare provider before making medication changes.
Results
Recommended Digoxin Dose: - mg/day
Amiodarone increases digoxin levels by 40-100%. Reduce by 50% immediately.
Recommended Warfarin Dose: - mg/day
Amiodarone increases warfarin effect by 30-50%. Reduce before starting amiodarone.
Critical Safety Information
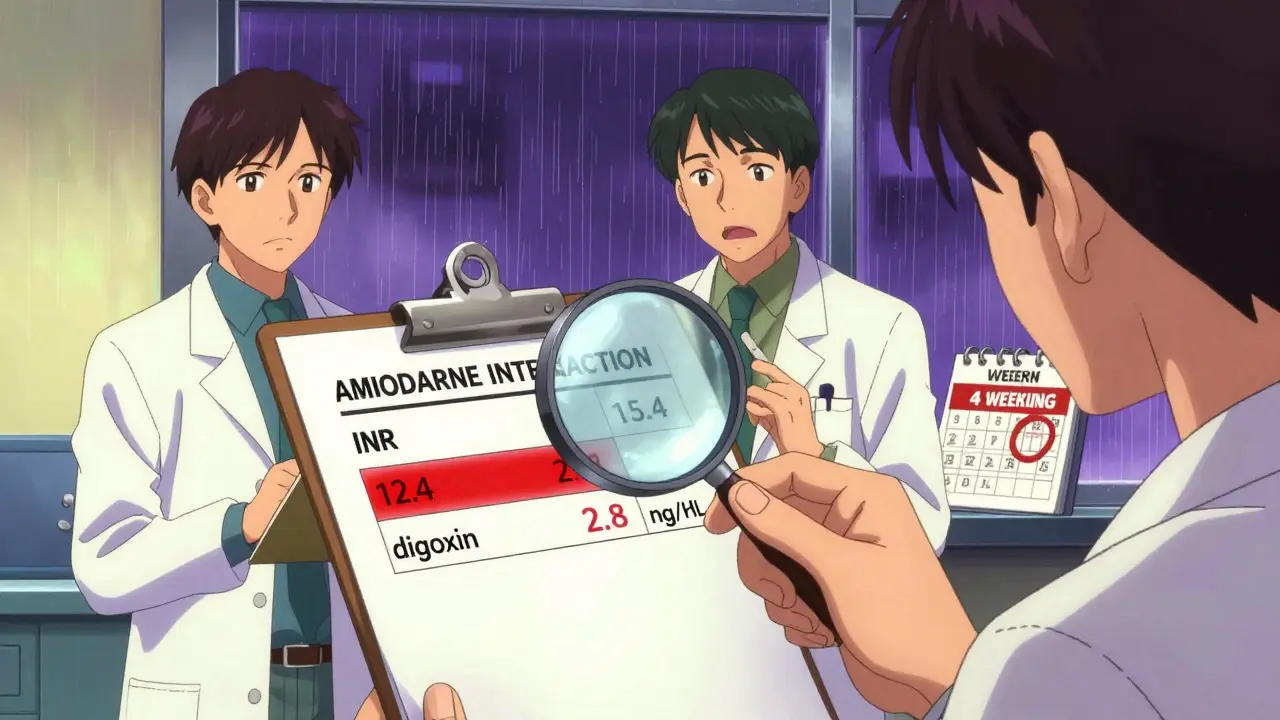
Always monitor digoxin levels (target < 1.2 ng/mL for patients over 70) and INR (check every 48-72 hours for first 2 weeks). Amiodarone's effects can last 4-6 weeks after discontinuation. Never adjust doses without consulting your doctor or pharmacist.
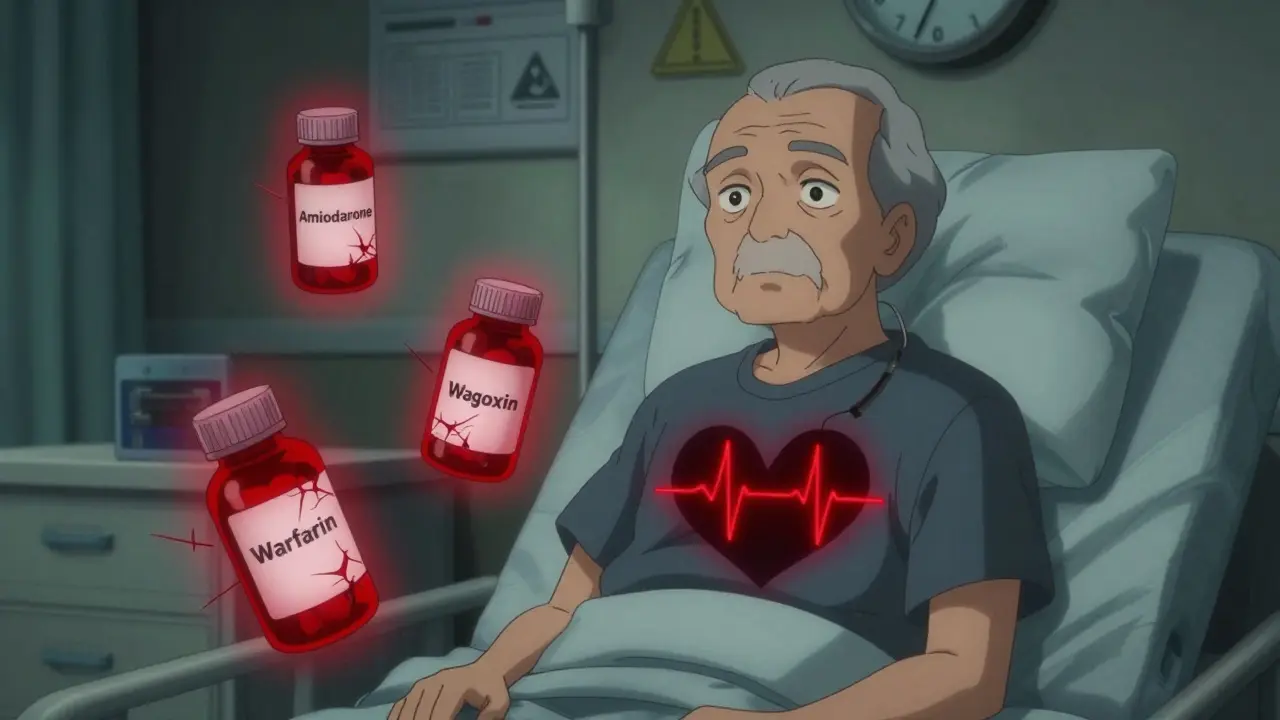
When three common heart drugs are taken together-amiodarone, digoxin, and warfarin-the result isn’t just a complicated prescription. It’s a ticking time bomb. This isn’t theoretical. It’s happening in hospitals, clinics, and living rooms across the country. Every year, thousands of patients are put at risk because this interaction is either missed, underestimated, or ignored. And when it goes wrong, it doesn’t just cause side effects-it causes death.
Why This Triad Is So Dangerous
Amiodarone is a powerful antiarrhythmic. It’s used to treat life-threatening heart rhythm problems like atrial fibrillation and ventricular tachycardia. Digoxin slows the heart rate in atrial fibrillation and helps the heart pump more efficiently in heart failure. Warfarin thins the blood to prevent strokes in people with irregular heart rhythms. Individually, each drug saves lives. Together? They turn each other into something far more dangerous. The problem starts with how amiodarone changes how the body handles the other two drugs. Amiodarone doesn’t just interact-it amplifies. It blocks the proteins that normally flush digoxin out of the body. This causes digoxin levels to spike by 40% to 100% within days. A dose that was perfectly safe yesterday can become toxic today. At the same time, amiodarone shuts down the liver enzymes (CYP2C9 and CYP3A4) that break down warfarin. This means warfarin sticks around longer, and its blood-thinning effect skyrockets. In one study, patients on this combo saw their INR-a measure of blood clotting time-jump from a safe 2.5 to over 6.0 in under two weeks. That’s not just elevated. That’s emergency room territory. And here’s the worst part: amiodarone sticks around for months. Even after you stop taking it, the drug and its metabolites linger in fat tissue, slowly leaking back into the bloodstream. So if you stop amiodarone, the interaction doesn’t vanish. It lingers. For weeks. Sometimes over a month. That means the risk doesn’t end when the pill bottle is empty.What Happens When Things Go Wrong
Digoxin toxicity doesn’t show up as a single symptom. It creeps in. Nausea. Vomiting. Dizziness. Blurry yellow vision. Then, if it’s not caught, the heart starts misfiring. Ventricular tachycardia. Cardiac arrest. In one case report, a 66-year-old man on all three drugs had his INR hit 12.4. He bled internally. He needed four units of plasma and a massive dose of vitamin K just to survive. Warfarin over-anticoagulation is just as brutal. A simple fall can lead to a brain bleed. A minor cut won’t stop bleeding. And because these patients are often elderly, with thin skin and fragile bones, even small injuries become life-threatening. A 2022 study found that patients on this triad had an 180% higher risk of major bleeding than those on warfarin alone. And the mortality rate? 28% higher than those taking digoxin without amiodarone. The FDA recorded 2,147 serious adverse events and 387 deaths linked to this triad in 2022 alone. That’s not a glitch. That’s a pattern. And it’s happening because doctors and pharmacists still don’t always see it coming.How to Prevent a Disaster
If you’re on any two of these drugs and your doctor wants to add the third, ask these questions:- Can we use a different rhythm drug instead of amiodarone? (Like dofetilide or dronedarone? They’re less risky.)
- Could we switch from warfarin to a DOAC like apixaban or rivaroxaban? (They’re not affected by amiodarone nearly as much.)
- If we must use all three, what’s the exact plan for dose changes and monitoring?
- Reduce digoxin by 50% the moment amiodarone starts. Don’t wait. Don’t assume it’s fine.
- Check serum digoxin levels 72 hours after starting amiodarone. If it’s above 1.2 ng/mL in someone over 70, it’s too high.
- Reduce warfarin by 30-50% before even starting amiodarone. Then monitor INR every 48-72 hours for the first two weeks.
- Keep checking INR weekly for at least four weeks after stopping amiodarone. It doesn’t disappear just because you stopped taking it.
Who’s Most at Risk
This isn’t a problem for young, healthy people. It’s almost always older adults with multiple heart conditions. The average patient in these cases is over 75. Many have kidney problems, which makes digoxin clearance even slower. Many are on other meds too-statins, antibiotics, even over-the-counter painkillers-that can make things worse. The data shows it: 63% of emergency cases involving this triad involved patients over 75 who had fallen. A hip fracture. A head injury. A brain bleed. All preventable if the drug interaction had been managed properly. And here’s something few realize: genetics play a role. Some people have a genetic variation in the P-glycoprotein transporter (ABCB1 gene). If you’re a TT homozygote, amiodarone can raise your digoxin level by 92%. If you’re CC? Only 58%. That means two people on the same dose can have wildly different outcomes.The Changing Landscape
The good news? Newer anticoagulants-DOACs like apixaban, dabigatran, and rivaroxaban-are replacing warfarin in most new atrial fibrillation cases. In 2022, 82% of new patients started on DOACs instead of warfarin. That’s a huge shift. And most DOACs aren’t affected by amiodarone the same way warfarin is. But here’s the catch: if you’ve been on warfarin for years because you have a mechanical heart valve, you can’t switch. And if you’re on digoxin because your heart is weak, you might not have alternatives. That means this triad isn’t going away. In fact, the American Heart Association predicts 4.3 million Americans will still be on this dangerous combo by 2030.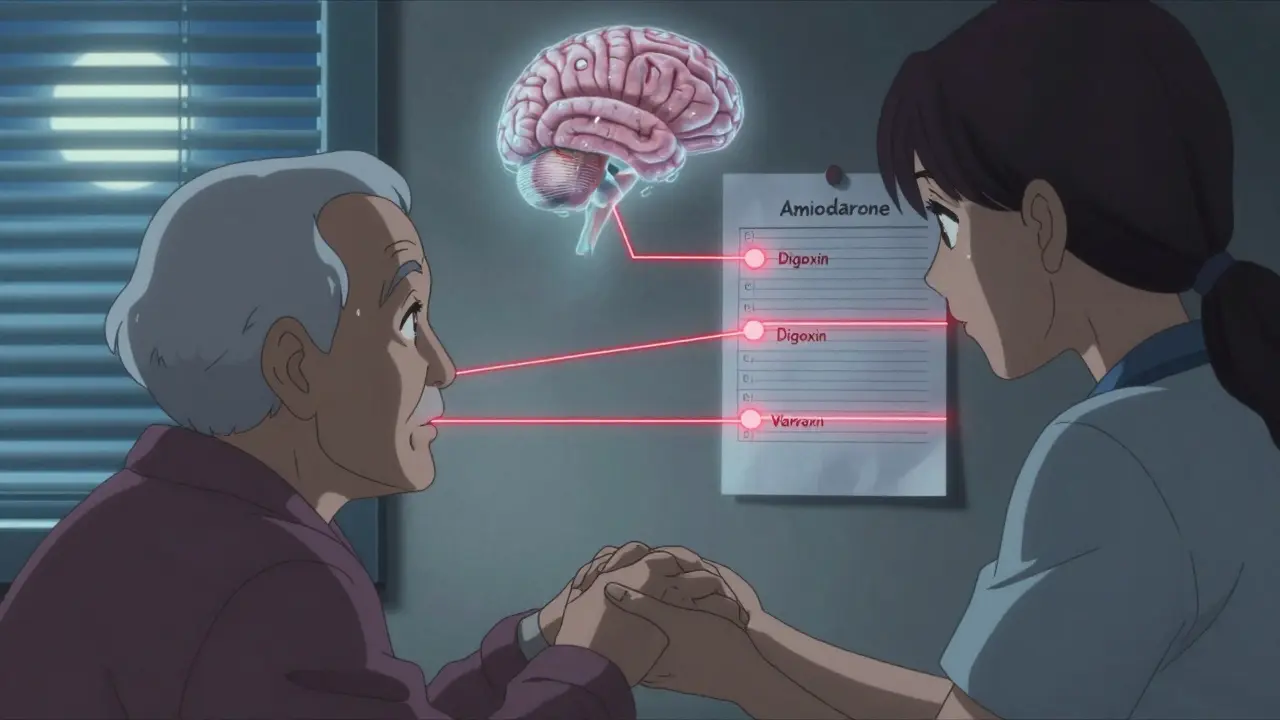
What You Need to Do
If you’re taking any of these three drugs:- Know your digoxin level. Ask for a blood test. Don’t wait until you feel sick.
- Know your INR. Keep a log. If it jumps more than 0.5 points in a week, call your doctor.
- Never stop or change a dose without talking to your pharmacist or cardiologist.
- Carry a list of all your meds-including supplements and OTC drugs-to every appointment.
Final Reality Check
This isn’t a rare edge case. It’s a common, preventable disaster. The science is clear. The guidelines are clear. The data is clear. Yet, this interaction still catches clinicians off guard. Why? Because we focus on the disease, not the drugs. Because we assume "if it’s been prescribed, it’s safe." It’s not. Not when amiodarone is in the mix. The truth is, this triad is one of the most dangerous combinations in all of cardiology. And if you’re on it, you’re not just managing a heart condition-you’re managing a minefield. Awareness isn’t optional. It’s survival.Can I take amiodarone with digoxin if I don’t take warfarin?
Yes, but it’s still risky. Even without warfarin, amiodarone can raise digoxin levels by up to 100%, leading to toxicity. The 2021 Circulation: Arrhythmia and Electrophysiology study found a 23% higher death rate in patients on amiodarone and digoxin compared to digoxin alone. Dose reduction and close monitoring are still required.
How long does the interaction last after stopping amiodarone?
Amiodarone has an extremely long half-life-25 to 100 days. Its effects on digoxin and warfarin can persist for 4 to 6 weeks after discontinuation. INR and digoxin levels must be monitored weekly during this time. Many patients are discharged without this warning, which leads to dangerous delays in dose adjustments.
Are there safer alternatives to this drug combo?
Yes. For arrhythmia control, dofetilide or dronedarone may be used instead of amiodarone. For anticoagulation, DOACs like apixaban or rivaroxaban are much safer than warfarin when combined with amiodarone. For rate control in atrial fibrillation, beta-blockers like metoprolol or calcium channel blockers like diltiazem are preferred over digoxin unless the patient has heart failure.
Why is digoxin still used if it’s so risky?
Digoxin is still used because it works well in patients with heart failure and atrial fibrillation, especially when other drugs like beta-blockers aren’t enough. It’s also cheap and available everywhere. But its narrow therapeutic window and high interaction risk mean it should only be used when absolutely necessary-and always with strict monitoring.
Can I check my digoxin level at home?
No. Digoxin levels require a blood test done in a lab. There are no home test kits available. If you’re on amiodarone and digoxin, your doctor should schedule a blood test within 72 hours of starting amiodarone and then weekly until levels stabilize. Don’t wait for symptoms to appear.
What should I do if I miss a dose of amiodarone?
Don’t double up. Missing a dose won’t immediately reverse the interaction, because amiodarone builds up in tissues. But irregular dosing can destabilize your heart rhythm. Contact your doctor or pharmacist immediately. They may need to adjust your digoxin or warfarin dose based on how long you’ve missed.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.