When someone on blood thinners suffers a serious bleed-like a fall that causes a brain hemorrhage-time isn’t just important, it’s life or death. These medications, called anticoagulants, keep clots from forming, but they also mean even a small injury can turn deadly. That’s where reversal agents come in. They’re not magic pills. They’re targeted, fast-acting tools designed to shut down the anticoagulant effect within minutes. If you’re a patient, a family member, or even a healthcare worker, understanding these agents isn’t just helpful-it’s essential.
Why Reversal Agents Matter
Every year, millions of people take blood thinners like warfarin, rivaroxaban, or apixaban. In the U.S. alone, about 4 million people rely on them. But when a major bleed happens, especially in the brain, the death rate jumps to 30-50%. That’s not a statistic-it’s someone’s parent, sibling, or neighbor. The goal isn’t to stop anticoagulation forever. It’s to stop it fast enough to save a life. Reversal agents do exactly that: they neutralize the drug’s effect so the body can start clotting again.
Not all reversal agents work the same way. Some are old and cheap. Others are new, expensive, and highly specific. Choosing the right one depends on which blood thinner the patient is on, how bad the bleed is, and what’s available at the hospital. There’s no one-size-fits-all solution.
Vitamin K: The Old Workhorse
Vitamin K has been around since the 1940s. It’s simple, cheap, and widely available. But it’s slow. If you give it intravenously, it takes 4-6 hours just to start working. Full reversal? That can take up to 24 hours. That’s too long when someone is bleeding out.
Its only job is to reverse warfarin and other vitamin K antagonists (VKAs). It doesn’t touch newer drugs like rivaroxaban or dabigatran. Vitamin K works by helping the liver make clotting factors again-factors II, VII, IX, and X. But here’s the catch: if you give vitamin K alone, you’re leaving the patient vulnerable for hours. That’s why it’s always paired with something faster, like PCC. Without it, the clotting factors that PCC gives you will disappear within hours, and the warfarin effect will come roaring back.
Prothrombin Complex Concentrate (PCC): The Go-To Bridge
PCCs are like a quick shot of clotting factors. Modern 4-factor PCCs contain factors II, VII, IX, and X, plus proteins C and S. They’re given as an IV infusion and start working in 15-30 minutes. For warfarin reversal, doctors use a simple dosing guide: 25-50 units per kg based on how high the INR is. For INR over 6, it’s 50 units/kg. That’s it.
PCCs aren’t perfect. They don’t reverse direct oral anticoagulants (DOACs) like apixaban or dabigatran. But here’s the twist: many emergency departments use PCCs off-label for DOACs anyway. Why? Because they’re cheaper and more available than the newer agents. A 2022 survey of 127 emergency rooms found that 63% of staff were comfortable using PCC for DOAC bleeds when specific reversal agents weren’t on hand.
And yes, it works. One 2018 study showed PCC corrected INR to under 1.5 in 92% of cases within 30 minutes-far faster than fresh frozen plasma (FFP), which only worked in 65%. But PCC isn’t risk-free. It can cause clots. About 8% of patients on PCC develop thromboembolic events like stroke or heart attack. Still, it’s often the best option when time and resources are tight.
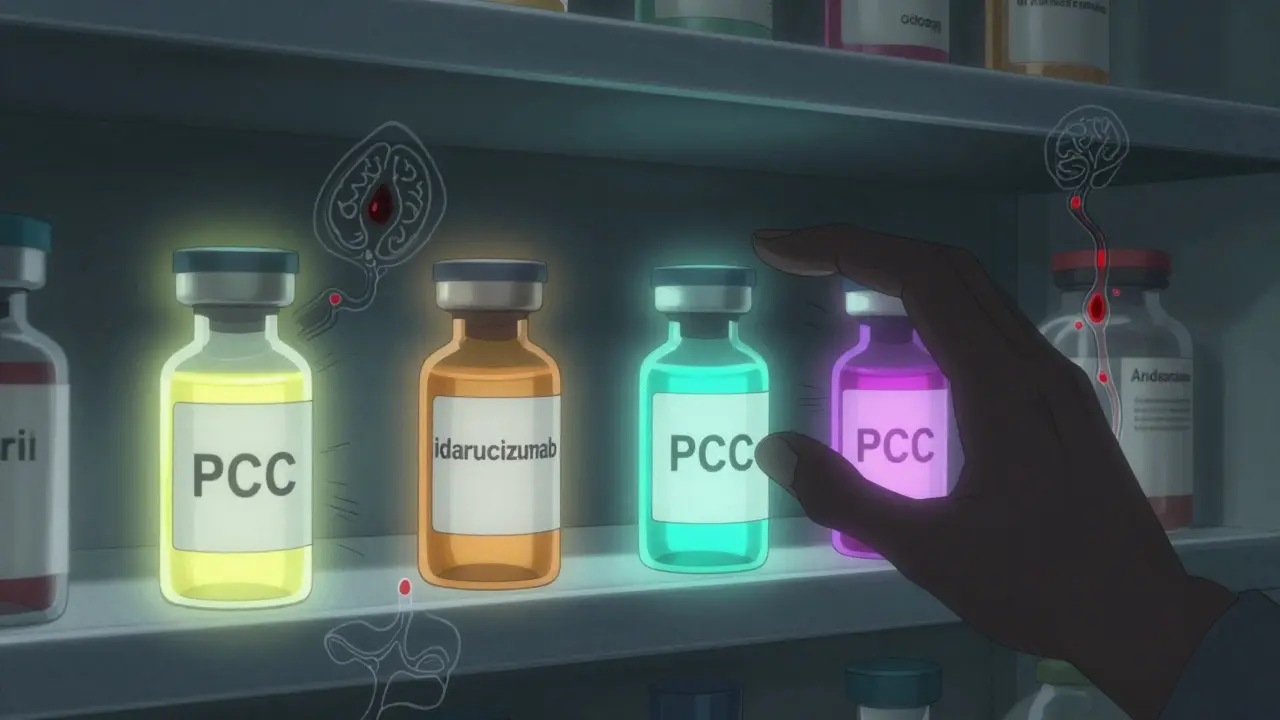
Idarucizumab: The Dabigatran Killer
Idarucizumab is a monoclonal antibody fragment. Sounds fancy, but it’s simple in practice. It binds to dabigatran like a magnet and pulls it out of circulation. No guesswork. No waiting. Within 5 minutes, the anticoagulant effect of dabigatran is gone. The RE-VERSE AD trial in 2015 showed 100% reversal of dabigatran’s effect in most patients.
It’s given as two 2.5g IV infusions-total 5g. That’s it. No dosing charts. No weight calculations. Just two bags, one after the other. It’s so straightforward, emergency teams in Australia and the U.S. now train new staff on it in under 15 minutes. And it’s safe. Thrombotic events? Only 5% in studies. That’s half the rate of PCC.
Cost? About $3,500 per dose. Not cheap, but far less than the alternatives. And availability? Nearly universal. Most hospitals keep it on the shelf. In fact, a 2022 survey found 78% of emergency departments preferred idarucizumab for dabigatran reversal. Why? Speed, simplicity, and safety.
Andexanet Alfa: Fast, Expensive, Risky
Andexanet alfa is designed for the newer factor Xa inhibitors: rivaroxaban, apixaban, and edoxaban. It works by acting like a decoy. The drug binds to factor Xa inhibitors instead of your body’s natural clotting factors, freeing up your own system to clot again.
The dosing is complex: a 400mg IV bolus, followed by a 4mg/min infusion for 120 minutes. It works in 2-5 minutes. That’s fast. But here’s the problem: its half-life is only about an hour. If the patient’s original drug is still in their system, the anticoagulant effect can return. That means redosing might be needed-and that’s not always clear in practice.
And then there’s the risk. In the ANNEXA-4 trial, 14% of patients had serious clotting events-stroke, heart attack, pulmonary embolism. That’s nearly double the rate of PCC. The FDA even added a boxed warning about this. The cost? $13,500 per treatment. Only 65% of U.S. hospitals stock it. Why? It’s expensive, complicated to use, and the data doesn’t clearly show it’s better than PCC for survival.
Some experts, like Dr. Samuel Z. Goldhaber, have said there’s “no convincing evidence” that andexanet alfa is superior to PCC for general bleeding. Yet, because it’s marketed as the “specific” reversal agent, it’s often used by default-even when PCC would do the job.

Which One Do You Choose?
Let’s break it down:
- Warfarin? Use 4F-PCC + vitamin K. Don’t skip the vitamin K. It prevents rebound bleeding.
- Dabigatran? Idarucizumab. Fast, safe, simple. Worth every dollar.
- Rivaroxaban or Apixaban? If you have andexanet alfa, use it. If not, 4F-PCC is a solid alternative. Don’t wait for the expensive option if it’s not available.
Cost matters. A lot. A single dose of andexanet alfa could pay for 10 doses of PCC. In many hospitals, especially outside big cities, PCC is the only option. And it works. The 2024 ACCP guidelines say: “4F-PCC remains a viable alternative when specific agents are unavailable.” That’s not a compromise-it’s a proven strategy.
What’s Coming Next?
There’s a new player on the horizon: ciraparantag. It’s a synthetic molecule that can reverse all anticoagulants-warfarin, heparin, and all DOACs. Phase III trials are wrapping up, and FDA approval could come by late 2025. Imagine one drug for every situation. That’s the dream.
But until then, we work with what we have. And the truth is, we have good options. The best reversal agent isn’t the newest or the most expensive. It’s the one you have, know how to use, and can give fast.
For patients: if you’re on blood thinners, know which one you take. Ask your doctor what reversal agent would be used if you had a bleed. Keep a card in your wallet with your medication and dose.
For providers: train your team. Have protocols. Stock the right drugs. Don’t wait for a crisis to learn how to use them.
Reversal isn’t about perfection. It’s about speed, safety, and readiness.
Can vitamin K reverse all types of blood thinners?
No. Vitamin K only works on warfarin and other vitamin K antagonists. It has no effect on direct oral anticoagulants (DOACs) like rivaroxaban, apixaban, or dabigatran. Using vitamin K for these drugs will not help and delays proper treatment.
Is PCC safe for reversing DOACs even though it’s off-label?
Yes. While 4F-PCC isn’t officially approved for reversing DOACs, it’s widely used and supported by clinical evidence. Studies show it can effectively reduce bleeding in patients on rivaroxaban or apixaban, especially when specific reversal agents aren’t available. Many emergency departments rely on it as a first-line option.
Why is andexanet alfa associated with more clots than other agents?
Andexanet alfa works by flooding the bloodstream with factor Xa-like proteins. This can trigger the body’s clotting system too aggressively, especially in patients who already have risk factors like recent surgery, atrial fibrillation, or a history of clots. The ANNEXA-4 trial found 14% of patients had thrombotic events, leading to an FDA boxed warning. It’s effective but carries higher risk than idarucizumab or PCC.
How quickly does idarucizumab work compared to andexanet alfa?
Both work fast, but idarucizumab is slightly faster and more predictable. Idarucizumab reverses dabigatran within 5 minutes. Andexanet alfa reverses factor Xa inhibitors in 2-5 minutes. However, idarucizumab’s effect is immediate and lasts longer, while andexanet alfa’s effect fades quickly (half-life ~1 hour), sometimes requiring redosing.
Do all hospitals carry these reversal agents?
No. Vitamin K and 4F-PCC are available in nearly all hospitals. Idarucizumab is stocked in most major centers. Andexanet alfa is only in about 65% of U.S. hospitals due to its high cost and complex storage needs. Rural and smaller hospitals often don’t have it. That’s why protocols using PCC are critical.
What’s the best reversal strategy for a patient on apixaban with a brain bleed?
If available, use andexanet alfa. If not, give 4F-PCC at 50 units/kg immediately, followed by vitamin K. Delaying treatment to wait for andexanet alfa can be deadly. PCC is proven, fast, and saves lives when the specific agent isn’t on hand.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.