Anticoagulant Bleeding Risk Calculator
Personal Risk Assessment
Getting prescribed a blood thinner can feel like walking a tightrope. On one side, you’re protected from deadly clots-strokes, heart attacks, pulmonary embolisms. On the other, you’re at risk of bleeding that can turn life-threatening in minutes. This isn’t theoretical. Every year, 1 in 50 people on anticoagulants ends up in the hospital because of uncontrolled bleeding. The good news? Most of these events are preventable. It’s not about avoiding medication-it’s about managing it smartly.
Why Blood Thinners Are Necessary (and Dangerous)
Anticoagulants don’t actually thin your blood. They slow down the clotting process. That’s critical if you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis. Without them, clots can form in your heart or veins, break loose, and block blood flow to your brain or lungs. But the same mechanism that stops dangerous clots can also cause dangerous bleeding. The most common anticoagulants fall into three groups: warfarin, heparin derivatives, and direct oral anticoagulants (DOACs). Warfarin has been around since the 1950s. It’s cheap-about $4 a month-but it needs constant monitoring. Your INR (International Normalized Ratio) must stay between 2.0 and 3.0 for most conditions. If it drops below 2.0, your clot risk rises. If it climbs above 3.0, your bleeding risk spikes. Studies show that every 10% drop in the time you spend in that ideal range increases your chance of major bleeding by 15%. DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban changed the game. They don’t need routine blood tests. Dosing is fixed. But they’re not perfect. They cost $500 a month without insurance. And until recently, reversing their effects in an emergency was nearly impossible. Now we have antidotes, but they’re expensive-$13,000 per dose for andexanet alfa, which reverses apixaban and rivaroxaban. Dabigatran has idarucizumab, a $3,000 antidote. These aren’t just drugs-they’re high-stakes tools.Who’s at Highest Risk for Bleeding?
Not everyone on anticoagulants bleeds. But some people are far more vulnerable. Age is the biggest factor. If you’re over 75, your risk of major bleeding is two to three times higher than someone under 65. Why? Kidneys slow down. Liver function declines. Medications pile up. Even a small dose of a DOAC can become toxic if your kidneys can’t clear it. Renal function matters more than you think. Apixaban requires a dose reduction if your creatinine clearance (CrCl) falls below 25 mL/min. Rivaroxaban needs adjustment below 50 mL/min. Edoxaban and dabigatran have similar thresholds. Many doctors check kidney function once at the start and forget about it. That’s a mistake. If your CrCl drops from 60 to 40 over six months, your drug levels are rising-slowly, silently, dangerously. Another major risk factor? Taking other drugs that affect bleeding. Aspirin, clopidogrel, NSAIDs like ibuprofen or naproxen-even some herbal supplements like fish oil, ginkgo, or garlic-can double or triple your bleeding risk. A 2019 study found that patients on both warfarin and an antiplatelet had a 70% higher chance of serious bleeding than those on warfarin alone. The same applies to DOACs. If you’re on apixaban and take ibuprofen for back pain, you’re playing Russian roulette with your blood vessels.
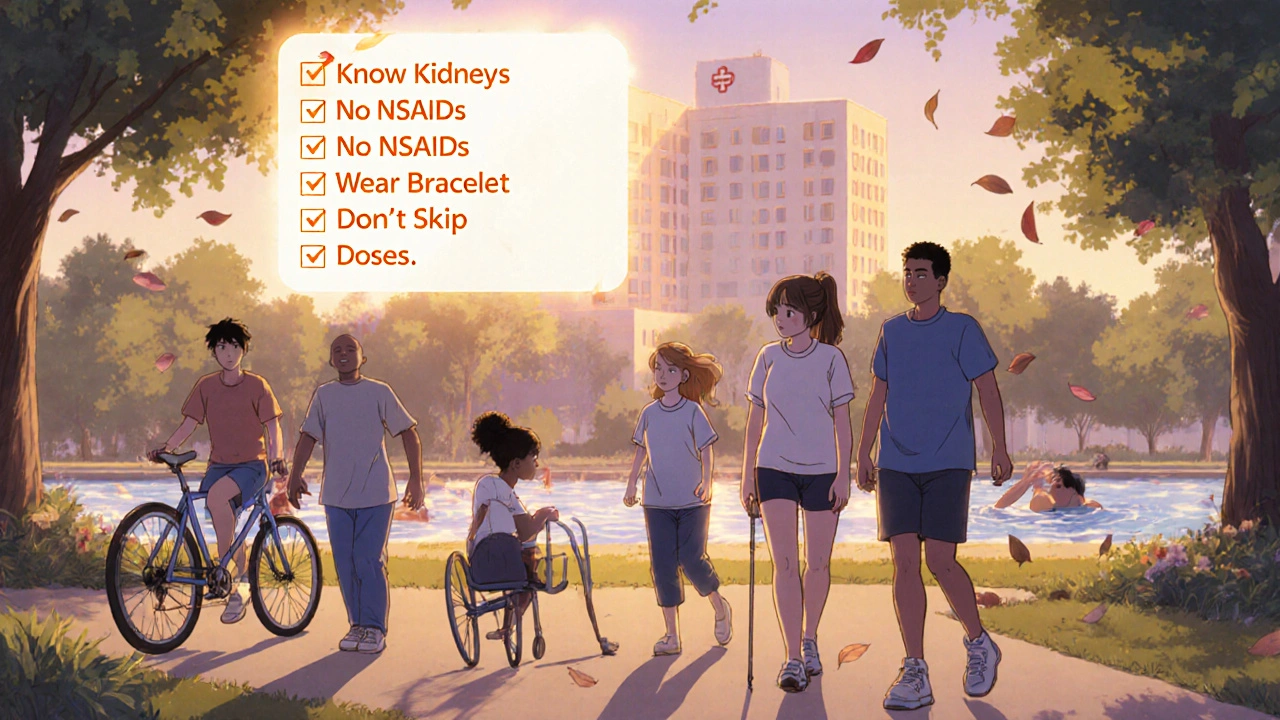
How to Prevent Bleeding: The Real-World Checklist
Preventing hemorrhage isn’t about avoiding activity. It’s about reducing avoidable risks. Here’s what works:- Know your kidney numbers. Get a CrCl test every 3-6 months if you’re stable. If you’re over 75 or have diabetes, do it every 3 months. Don’t wait for symptoms.
- Avoid NSAIDs. Use acetaminophen (Tylenol) for pain. No ibuprofen, no naproxen. Even occasional use raises bleeding risk.
- Stop dual therapy unless absolutely necessary. If you’re on a DOAC and aspirin for heart disease, ask your doctor if you can drop the aspirin. Most people don’t need both.
- Don’t skip doses or double up. If you miss a dose of apixaban, take it within 6 hours. If it’s been longer, skip it. Never double the next dose. Same for rivaroxaban. Overdosing is a leading cause of ER visits.
- Use a pill organizer. Especially if you take multiple meds. Confusion between warfarin and DOACs is common. One wrong pill can cause a bleed.
- Wear a medical alert bracelet. It says “ON ANTICOAGULANT” and lists your drug. Emergency staff don’t have time to guess.
- Know your reversal agents. If you’re on warfarin, 4f-PCC can reverse it in 15 minutes. If you’re on apixaban, andexanet alfa is the antidote. Ask your doctor to write down what to do in an emergency-and keep that note in your wallet.
What to Do If You Bleed
Not every bruise is an emergency. But some signs mean you need help now:- Bleeding that won’t stop after 10 minutes of pressure
- Bright red blood in stool or black, tarry stools
- Vomiting blood or coffee-ground material
- Sudden, severe headache with dizziness or vision changes
- Unexplained swelling or pain in joints or muscles
- Heavy menstrual bleeding (soaking through a pad every hour)
When to Restart After a Bleed
Many patients stop their anticoagulant after a bleed-out of fear. That’s often the worst thing you can do. Stopping increases your risk of stroke or clot-related death more than continuing does. The American College of Cardiology recommends restarting anticoagulation as soon as it’s safe. For someone with atrial fibrillation and a CHA₂DS₂-VASc score of 4 or higher, restarting within 7-14 days after a minor bleed (like a nosebleed or bruise) is standard. For major bleeds-like a brain hemorrhage or GI bleed-you wait longer. But you don’t quit. Studies show that patients who restart anticoagulation after a major bleed have a 50% lower risk of death over the next year than those who don’t. The key is timing and risk assessment. Your doctor should use tools like HAS-BLED to weigh your bleeding risk against your clot risk-not just guess.The Future: Better Tools, Fewer Bleeds
The next big breakthrough isn’t a new drug-it’s better monitoring. Right now, there’s no quick way to check if your DOAC level is too high. Unlike INR for warfarin, there’s no simple blood test you can get at a clinic. But that’s changing. Several point-of-care tests for DOACs are in late-stage trials. These could give you a result in 10 minutes, like a glucose meter. Imagine checking your rivaroxaban level before surgery or after a fall. That could prevent 15-20% of emergency bleeds. There’s also ciraparantag, a universal antidote in development. If it works, one drug could reverse all DOACs and even heparin. That would be a game-changer for ER teams. For now, the best tool you have is knowledge. Know your drug. Know your kidneys. Know your risks. And never assume your doctor knows everything about your meds. Ask questions. Keep records. Be your own advocate.Can I still exercise while on blood thinners?
Yes-but avoid high-risk activities. Walking, swimming, cycling, and light strength training are safe. Avoid contact sports like football or boxing, and activities with high fall risk like rock climbing or skiing without proper protection. Even a minor bump can cause internal bleeding. Talk to your doctor about your routine.
Do I need to change my diet if I’m on a DOAC?
No, not like with warfarin. Warfarin interacts with vitamin K-rich foods like kale, spinach, and broccoli. DOACs don’t. You can eat these foods normally. But avoid massive, sudden changes in your diet. A sudden jump in leafy greens won’t affect apixaban, but it might confuse your doctor if you’re also on warfarin.
Is it safe to get dental work done on blood thinners?
Almost always yes. Most routine dental procedures-cleanings, fillings, even extractions-can be done safely without stopping anticoagulants. The risk of a clot from stopping is greater than the risk of bleeding from the procedure. Your dentist may use sutures or hemostatic agents to control bleeding. Never stop your medication without consulting your doctor.
What if I fall and hit my head?
Get checked-even if you feel fine. A head injury on anticoagulants can lead to a slow, silent brain bleed. Symptoms might not appear for hours or days. CT scans can detect bleeding early. Don’t wait for a headache. If you’re on warfarin or a DOAC and fall hard, go to the ER.
Can I drink alcohol while on anticoagulants?
Moderation is key. One drink a day is usually okay. More than that increases bleeding risk and can interfere with liver metabolism of warfarin. Alcohol also raises your chance of falls. If you drink regularly, tell your doctor. They may adjust your dose or recommend testing your INR more often.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.