When you roll over in bed and suddenly feel like the room is spinning, it’s not just dizziness. It’s BPPV - benign paroxysmal positional vertigo. This isn’t anxiety, it’s not a migraine, and it’s not something you just need to “shake off.” It’s a physical problem inside your inner ear, caused by tiny calcium crystals that got loose and are now sending wrong signals to your brain. The good news? You don’t need surgery, pills, or scans. There’s a simple, proven fix that works in minutes - and most people feel better after just one try.
What Exactly Is BPPV?
BPPV is the most common cause of vertigo in adults. That means if you’re feeling like you’re on a spinning ride, and it only happens when you move your head - like rolling over, looking up, or bending down - there’s a very good chance it’s BPPV. It’s not dangerous, but it’s intensely disruptive. Episodes last only seconds to a minute, but they can hit you multiple times a day. You might feel nauseous, lose your balance, or even vomit. Some people avoid sleeping on one side. Others stop driving because they fear an episode while turning their head.
The cause? Tiny crystals called otoconia. Normally, they sit safely in a part of your inner ear called the utricle, helping you sense gravity and head position. But sometimes, due to aging, head bumps, or just unknown reasons, they break loose. They drift into one of the three fluid-filled semicircular canals - most often the posterior canal. When you move your head, these crystals push on the fluid inside the canal, tricking your brain into thinking you’re spinning when you’re not. That’s the vertigo.
How Do Doctors Know It’s BPPV?
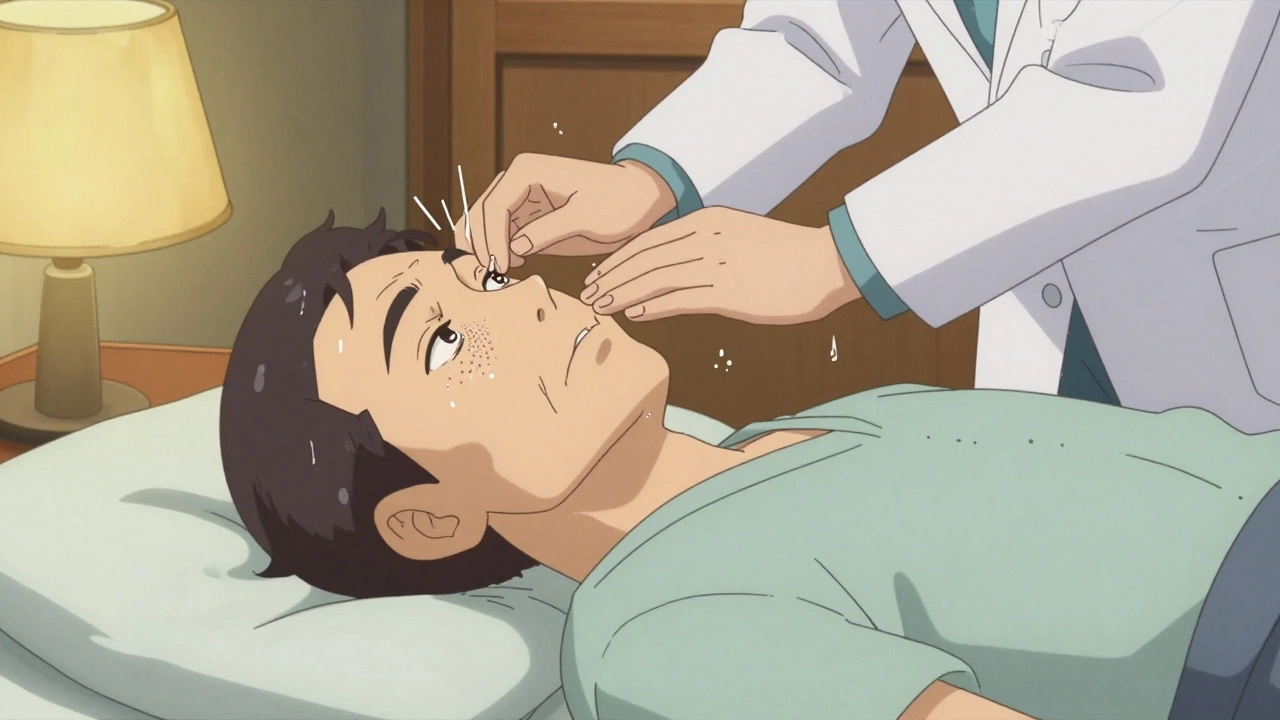
There’s no blood test. No MRI needed. In fact, MRIs often show nothing at all in BPPV cases - and they cost over $1,200. Instead, doctors use a simple test called the Dix-Hallpike maneuver. You sit on the edge of a table. The doctor turns your head 45 degrees to one side, then quickly lowers you backward, letting your head hang off the table. If you have BPPV, you’ll feel dizzy within a few seconds. Their eyes will also see a specific type of involuntary eye movement called nystagmus - the telltale sign.
This test is accurate about 80% of the time. And here’s the kicker: if you’ve had this kind of vertigo for more than a few days, and you’re over 50, and it only happens with head movement - you probably have BPPV. Studies show that over half of all vertigo patients seen by doctors actually have BPPV, but nearly a third are misdiagnosed as having migraines, anxiety, or inner ear infections.
Canalith Repositioning: The Real Cure
The treatment? Canalith repositioning. That’s just a fancy name for a series of head movements designed to move those loose crystals back where they belong. The most common version is the Epley maneuver. It’s done in a doctor’s office, but you can also do it at home with a video guide.
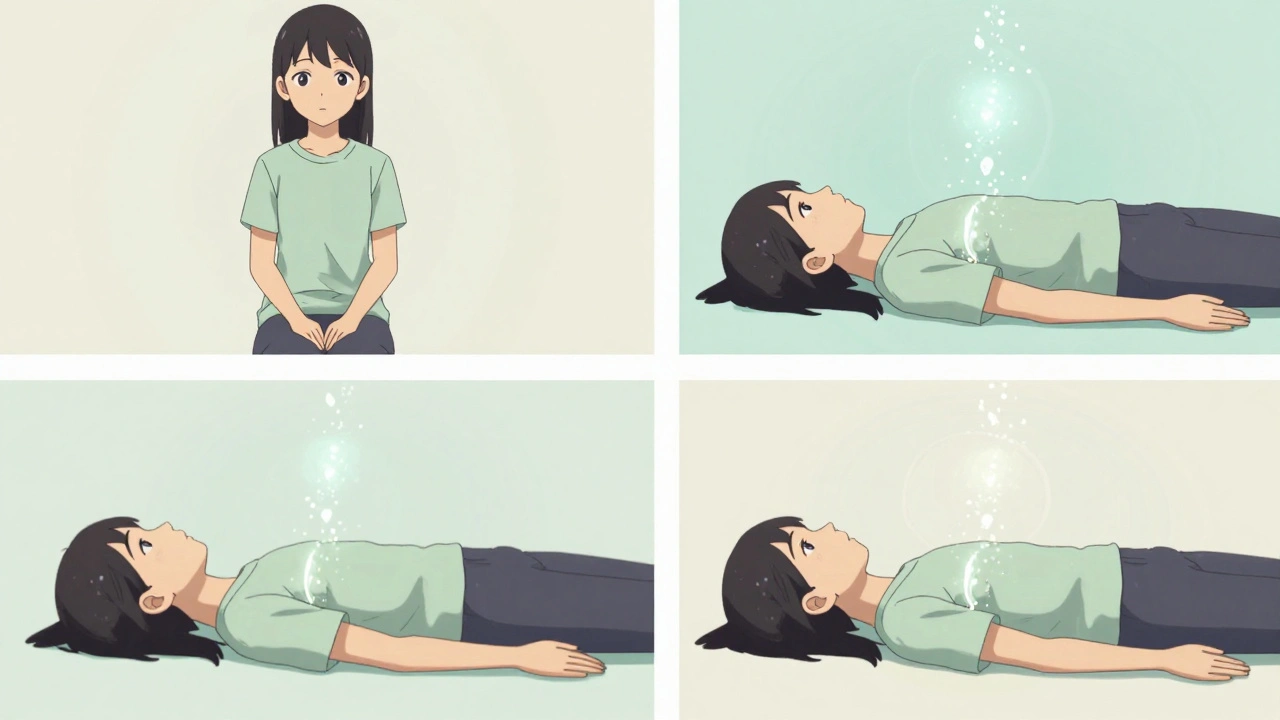
Here’s how the Epley maneuver works, step by step:
- You sit upright on a bed or table, with your legs stretched out.
- The doctor turns your head 45 degrees toward the side that triggers your dizziness.
- You lie back quickly, keeping your head turned, so your shoulders are on the bed but your head is hanging slightly off the edge.
- You wait 30 to 60 seconds - the dizziness should peak, then fade.
- You turn your head 90 degrees to the opposite side, without lifting it up.
- You wait another 30 to 60 seconds.
- You roll onto your side, facing the floor, so your nose is pointing down.
- You wait another 30 seconds.
- You sit up slowly, keeping your head turned slightly downward.
That’s it. One session. Takes about five minutes. Studies show it works in 80 to 90% of posterior canal BPPV cases. Most people feel better immediately. Some need two or three tries, especially if the crystals are stubborn or stuck in another canal.
What If It’s Not the Posterior Canal?
While 80-90% of BPPV cases involve the posterior canal, about 5-10% affect the horizontal canal. This type feels different - you get dizzy when you turn your head side to side, like checking over your shoulder. The fix is the Lempert roll (or barbecue roll), where you lie on your back and rotate your head 90 degrees left, then right, then left again, in a slow, controlled motion. It’s trickier to do on your own, so it’s usually done by a specialist.
There’s also the Semont maneuver, another repositioning technique that works almost as well as Epley. It’s faster - just two quick position changes - but some people find it more intense. Both are more effective than any medication.
Why Pills Don’t Work
Doctors used to prescribe drugs like meclizine or diazepam to “calm the inner ear.” But here’s the truth: those pills don’t fix BPPV. They just numb your symptoms. You might feel less dizzy for a few hours, but the crystals are still loose. Studies show these medications help only 18% of BPPV patients. Worse, they cause drowsiness, brain fog, and dry mouth - and they don’t stop the vertigo from coming back.
The American Academy of Otolaryngology says clearly: Don’t use vestibular suppressants for BPPV. The only thing that gets rid of the problem is moving the crystals. Medications are a distraction. They delay real treatment.
Can You Do It Yourself?
Yes. And many people do. YouTube has over 15 million views of Epley maneuver tutorials. Apps like DizzyFix use your phone’s motion sensors to guide you through the steps. A 2021 study in JAMA Otolaryngology found that people who followed a video guide at home had a 72% success rate. That’s nearly as good as seeing a specialist.
But here’s the catch: you have to do it right. If you move too fast, skip a step, or do it on the wrong side, it won’t work - or it might make things worse. If you’re unsure, start with a video from a trusted source: a university medical center, the Vestibular Disorders Association, or your ENT’s website. Don’t guess. And if you feel worse after trying it, stop and see a professional.

What Happens After Treatment?
Most people feel better right away. Some feel a little off for a day or two - that’s normal. Your brain is relearning what’s real. Avoid sudden head movements for 48 hours after the maneuver. Don’t lie flat on your back. Sleep propped up with pillows. Avoid looking up or bending over too far.
But BPPV loves to come back. About 15% of people have another episode within a year. By five years, it’s 35%. By ten years, it’s 50%. That doesn’t mean you’re broken. It just means your inner ear is prone to this. Some people get it every few years. Others get it once and never again.
There’s one promising new finding: low vitamin D levels are linked to higher recurrence rates. If you’ve had BPPV more than once, ask your doctor to check your vitamin D. Taking 1,000 IU daily may cut your risk of recurrence by nearly a quarter.
When to See a Doctor
You don’t need to panic if you feel dizzy. But if you have any of these, go to a doctor right away:
- Dizziness that lasts longer than a minute
- Headache, blurred vision, slurred speech, or weakness in your arms or legs
- Loss of hearing or ringing in your ears
- Dizziness after a head injury
These aren’t BPPV signs. They could point to something more serious - like a stroke or a tumor. BPPV is harmless. But if your vertigo comes with other symptoms, don’t assume it’s just BPPV.
What’s New in BPPV Treatment?
Technology is making diagnosis easier. Some clinics now use video goggles that record your eye movements automatically. That way, they don’t have to guess whether you have nystagmus - they can see it. There’s even a new FDA-approved virtual reality program that guides patients through repositioning exercises at home. It costs $300 per course, but it’s proven to reduce symptoms by 78%.
And while the Epley maneuver has been around since the 1980s, it’s still the gold standard. No drug, no surgery, no expensive machine beats it. It’s cheap, fast, safe, and effective. The real problem isn’t the treatment - it’s that most doctors still don’t know how to do it. A 2023 survey found that over half of primary care providers haven’t been trained in canalith repositioning. That’s why so many people wait months for the right diagnosis.
But that’s changing. More clinics are adding vestibular therapists. More medical schools are teaching the Dix-Hallpike test. And more patients are learning how to fix it themselves - safely and correctly.
If you’ve been living with vertigo, thinking it’s just part of getting older - it’s not. It’s BPPV. And it can be fixed. Today. Right now. You just need to know how.
Is BPPV the same as regular dizziness?
No. Regular dizziness is a general feeling of lightheadedness or unsteadiness. BPPV is a sudden, spinning sensation triggered only by specific head movements - like rolling over or looking up. It lasts seconds, not minutes or hours, and it’s caused by loose crystals in the inner ear, not low blood sugar, dehydration, or anxiety.
Can BPPV go away on its own?
Yes, sometimes. About 40-50% of cases resolve within a month without treatment. But waiting that long means you’ll have days - or weeks - of nausea, imbalance, and fear of movement. Canalith repositioning fixes it in minutes. Why wait?
How many times do I need to do the Epley maneuver?
Most people feel better after one session. About 30% need a second or third try, especially if the crystals are stuck in the canal or if they have BPPV in both ears. If you don’t improve after three attempts, you may have a different type of vertigo - and should see a specialist.
Can BPPV affect both ears?
Yes. About 15-20% of people have BPPV in both ears at the same time. That’s called bilateral BPPV. It’s less common but possible. If you get dizzy when turning your head left or right, it might be in both canals. A specialist can test each side separately and treat both.
Is the Epley maneuver safe for older adults?
Absolutely. BPPV is most common in people over 50, and the Epley maneuver is perfectly safe for seniors. In fact, it’s the preferred treatment because it avoids risky medications. Just go slow, use pillows for support, and have someone nearby the first time you try it at home.
What if the Epley maneuver doesn’t work?
If you’ve tried the Epley maneuver correctly two or three times with no improvement, you may have a different condition - like vestibular neuritis, Meniere’s disease, or even a neurological issue. See a vestibular specialist. They can do advanced tests and rule out other causes. Don’t keep trying the same thing if it’s not helping.
Can stress cause BPPV?
Stress doesn’t cause BPPV, but it can make symptoms feel worse. If you’re anxious, your brain is more sensitive to dizziness. That’s why many people with BPPV report increased symptoms during high-stress periods. Treating the physical cause (the crystals) is still the solution - but managing stress helps you recover faster.
Are there any long-term side effects of the Epley maneuver?
No. The Epley maneuver is non-invasive and has no known long-term side effects. Some people feel briefly nauseous or dizzy during the procedure - that’s normal. Rarely, the crystals might shift into another canal, causing a different type of vertigo. That’s why it’s best done by a trained professional the first time.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.