When your immune system turns against your own body, food isn’t just fuel-it becomes a tool. For people living with autoimmune diseases like rheumatoid arthritis, Hashimoto’s thyroiditis, or Crohn’s disease, what’s on the plate can mean the difference between a flare-up and a quiet day. This isn’t about miracle cures. It’s about science-backed ways to calm the fire inside.
What Anti-Inflammatory Eating Actually Means
Anti-inflammatory eating isn’t a fad. It’s not a 30-day cleanse or a juice detox. It’s a pattern of eating that focuses on whole, real foods that help reduce chronic inflammation-the silent driver behind most autoimmune conditions. Unlike medications that suppress the immune system, these diets work by supporting the body’s natural balance. Think of inflammation like a smoke alarm that won’t turn off. In autoimmune diseases, it’s going off even when there’s no fire. Anti-inflammatory diets don’t silence the alarm-they help fix the wiring. And the evidence is growing. A 2022 meta-analysis in the British Journal of Nutrition found that people following these diets saw CRP (a key inflammation marker) drop by 20-30% compared to those eating standard Western meals.The Diets That Actually Work
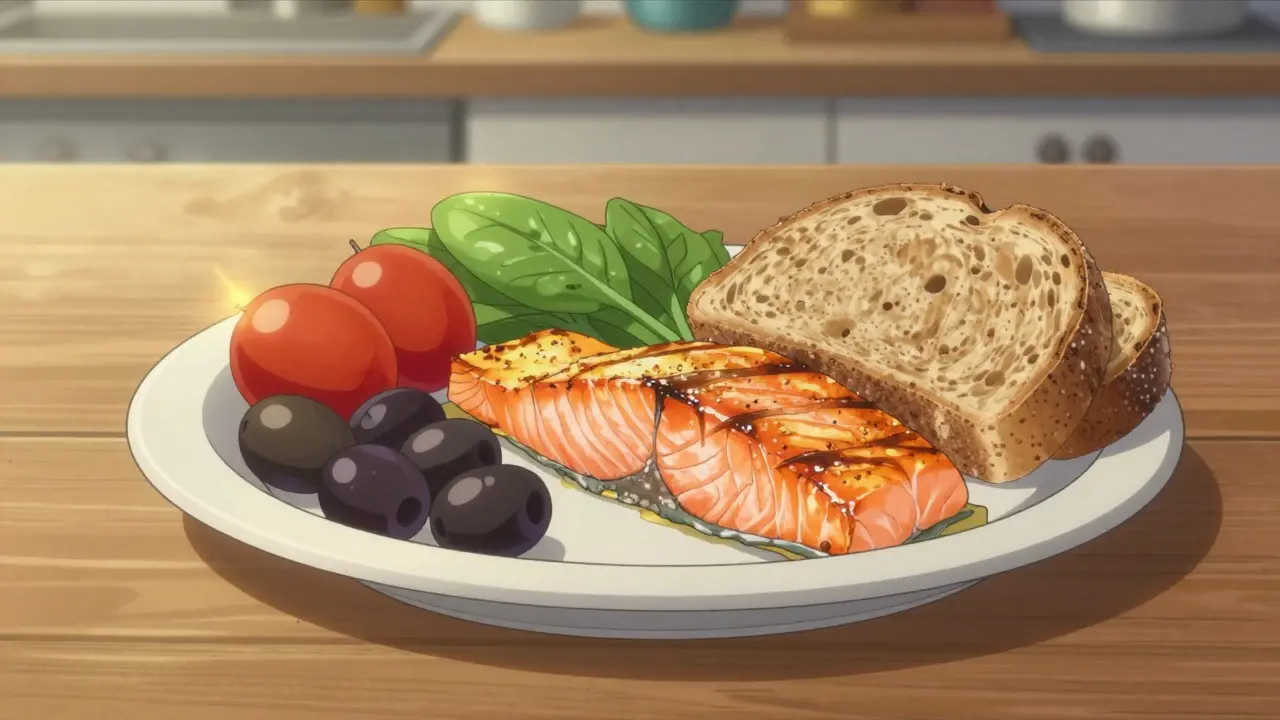
Not all anti-inflammatory diets are the same. Some are backed by decades of research. Others are newer, with promising but limited data. Here’s what the science says about the most studied patterns.The Mediterranean Diet is the gold standard. It’s not about eating olives and feta every day-it’s about daily servings of vegetables (7-10), whole grains (5-9), legumes (3-4 times a week), fatty fish (2-3 times a week), nuts, seeds, and extra virgin olive oil (at least 2 tablespoons). A 2021 trial with 2,500 people with rheumatoid arthritis showed a 22% drop in disease activity and 18% lower CRP levels after just one year. Adherence? Around 85% after six months. That’s high for any diet.
Vegetarian and Vegan Diets also show strong results. A review of 21,000 people found vegetarians had 26% lower CRP levels than omnivores-especially if they’d been on the diet for two years or more. The key? Fiber. Plant-based diets push fiber intake past 30g a day, which feeds good gut bacteria that produce butyrate-a compound linked to 20% lower levels of IL-6, another inflammation signal.
The Autoimmune Protocol (AIP) Diet is stricter. It removes grains, legumes, dairy, eggs, nuts, seeds, nightshades (like tomatoes and peppers), and coffee for 5-8 weeks. Then, you slowly add them back one at a time to see what triggers symptoms. It’s not easy. But in observational studies, 60-70% of people with Hashimoto’s or IBD reported symptom improvements. One person on Reddit wrote, “Eliminating nightshades cut my psoriatic arthritis pain in half.” That’s not anecdotal-it’s a pattern.
The Ketogenic Diet is the newest player. A 2023 study from UCSF showed that ketosis-when your body burns fat for fuel-produces a molecule called β-hydroxybutyrate (βHB). In mice with MS-like symptoms, βHB blocked the activation of harmful immune cells. Human trials are still small, but early results are promising. The catch? Only 45% of people stick with keto after six months. Fatigue during the first few weeks is common.
What to Avoid
The real enemy isn’t just what you eat-it’s what you’re eating too much of.- Refined sugar: More than 25g a day spikes inflammation. That’s less than one can of soda.
- Processed foods: Anything with a long list of unpronounceable ingredients. These often contain industrial seed oils, preservatives, and hidden sugars.
- Trans fats: Found in fried foods and margarine. They directly activate inflammatory pathways.
- Excess saturated fat: Not all fats are bad, but too much from red meat and processed meats can worsen inflammation.
The Western diet-high in these items-is linked to 30-50% higher CRP levels. That’s not a coincidence. It’s a direct link.
The Gut Connection
Your gut isn’t just for digestion. It’s your immune system’s command center. About 70% of immune cells live in the gut lining. When that lining gets damaged-by sugar, processed foods, or antibiotics-it leaks. That’s called “leaky gut,” and it’s thought to trigger autoimmune responses. Anti-inflammatory diets fix this by feeding good bacteria. Fiber from vegetables, legumes, and whole grains turns into short-chain fatty acids like butyrate. These molecules strengthen the gut barrier and calm immune overreactions. The 2023 UCSF study took this further. They found that βHB from ketosis didn’t just block immune cells directly-it made a gut bacterium called Lactobacillus murinus produce indole lactic acid (ILA), which then shut down the very cells causing inflammation. That’s not just diet. That’s microbiome medicine.Real People, Real Results
Science is one thing. Real life is another. In a 2022 survey of 1,247 people in an autoimmune Reddit community, 68% said their symptoms improved with dietary changes. Common reports:- “Morning stiffness dropped from two hours to 30 minutes after six weeks on the Mediterranean diet.”
- “IBD flares went from monthly to quarterly.”
- “I stopped needing prednisone every few months.”
But there’s a flip side. The same survey found:
- “AIP is impossible at family dinners.”
- “Keto made me exhausted for weeks.”
- “I spent $75 more a week on groceries.”
Cost and social pressure are real barriers. The USDA estimates anti-inflammatory eating costs $50-75 more per week than a standard diet. That’s not small change.
What Experts Say
Dr. Frank Hu from Harvard says the Mediterranean diet “significantly decreased inflammation markers”-but he’s careful to note that direct evidence for autoimmune diseases is still limited. Dr. Peter Turnbaugh, who led the UCSF ketosis study, calls the findings “really exciting” for future supplements that mimic the diet’s effects. Meanwhile, the European League Against Rheumatism (EULAR) says the evidence isn’t strong enough yet to recommend diets as standard care. That’s not a dismissal-it’s a call for more research.
How to Start (Without Overwhelm)
You don’t need to overhaul your life overnight.- Start with one change: Swap white bread for sourdough. Add a handful of spinach to your smoothie. Eat fish twice a week.
- Focus on what to add, not just what to cut: More veggies, more fiber, more omega-3s from salmon, sardines, or flaxseeds.
- Track symptoms: Keep a simple journal. Note energy, pain, digestion. Look for patterns over 4-8 weeks.
- Get professional help: A registered dietitian who knows autoimmune conditions can cut your trial-and-error time in half. Studies show 83% of people who worked with one stuck with the diet after a year. Only 42% did on their own.
If you’re considering AIP or keto, start with a 2-week trial. Don’t go all-in until you’ve tested how your body reacts.
The Future Is Personalized
Right now, we’re in the early days. But the direction is clear. Companies like Viome and Zoe are already using gut microbiome tests to recommend personalized diets for autoimmune patients. In five years, your diet plan might be based on your unique bacteria, not a generic template. The NIH is funding a major 5-year trial called DIETA, which will compare the Mediterranean diet to standard eating in 1,000 early rheumatoid arthritis patients. Results come in 2026. That could change guidelines forever.Bottom Line
There’s no single diet that works for everyone with autoimmunity. But there’s strong, consistent evidence that eating whole, unprocessed foods reduces inflammation, improves symptoms, and sometimes even reduces medication needs. The Mediterranean diet has the most proof. AIP works for many, but it’s hard to maintain. Keto shows promise but isn’t for everyone. Vegetarian diets are powerful-if you plan them right. What matters most isn’t perfection. It’s progress. One more vegetable. One less sugary snack. One more week of consistency. That’s how you rebuild your body from the inside out.Can diet really reverse autoimmune disease?
No diet can cure autoimmune disease. But strong evidence shows it can significantly reduce symptoms, lower inflammation markers, and sometimes reduce reliance on medications. Many people report fewer flares, less pain, and better energy. It’s about management, not reversal.
Is the AIP diet safe long-term?
The elimination phase of AIP is short-term (5-8 weeks). Long-term avoidance of entire food groups like nuts, seeds, eggs, and legumes can lead to nutrient gaps-especially fiber, healthy fats, and protein. Reintroduction is critical. Never stay in strict elimination mode without professional guidance.
Do I need to take supplements with an anti-inflammatory diet?
Not if you’re eating well. But many people benefit from omega-3 supplements (especially if they don’t eat fish), vitamin D (low levels are common in autoimmune patients), and B12 (especially on vegan diets). Always test your levels first. Don’t guess.
How long until I see results?
Some notice changes in 2-4 weeks-less swelling, better digestion, more energy. For deeper immune changes, like lower CRP or fewer flares, expect 8-12 weeks. Patience is key. This isn’t a quick fix.
Can I eat out or travel on an anti-inflammatory diet?
Yes, but it takes planning. Choose grilled fish or chicken with steamed vegetables. Ask for olive oil instead of butter. Skip sauces and dressings unless you know the ingredients. Bring snacks like nuts or fruit. It’s not impossible-just requires a little more thought.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.