Every year, over 21,000 people in the U.S. are diagnosed with esophageal cancer. The survival rate is alarmingly low-only 21% for all stages combined. Understanding your esophageal cancer risk starts with recognizing how chronic GERD can lead to serious complications. While GERD affects about 20% of Americans, only a small fraction develop esophageal cancer. However, catching early warning signs can make all the difference for those at higher risk.
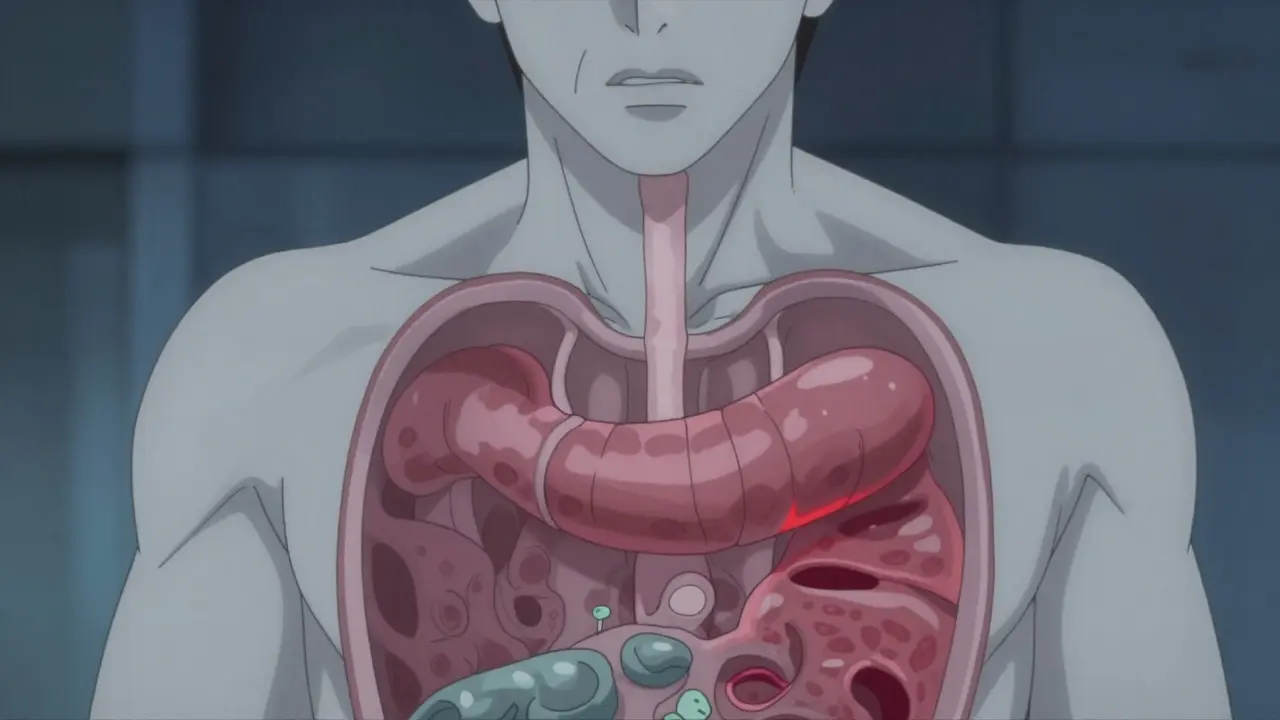
Esophageal Cancer is a malignancy that develops in the tissues of the esophagus, the muscular tube connecting the throat to the stomach. Chronic gastroesophageal reflux disease (GERD) is recognized as the strongest risk factor for esophageal adenocarcinoma, the most common type in the U.S. GERD (gastroesophageal reflux disease) happens when stomach acid frequently flows back into the esophagus. Occasional heartburn is normal, but chronic GERD-symptoms occurring at least twice a week for months or years-can damage the esophagus lining over time. This damage can lead to Barrett's Esophagus, where the normal cells in the esophagus change to resemble stomach cells. This change is the only known precursor to esophageal adenocarcinoma. According to a 2023 NIH study published in PMC, chronic GERD increases esophageal cancer risk by 3.2 times. However, only 0.5-2% of GERD patients develop Barrett's esophagus, and of those, just 0.2-0.5% per year progress to cancer.Key Risk Factors for Esophageal Cancer
| Risk Factor | Risk Increase | Notes |
|---|---|---|
| Male gender | 3-4 times higher risk | Men are 3-4 times more likely than women |
| Age over 50 | 90% of cases occur in people over 55 | Risk increases with age |
| White non-Hispanic ethnicity | 3 times higher adenocarcinoma rates | Compared to Black Americans |
| Obesity (BMI ≥30) | 2-3 times higher risk | Contributes to 30-40% of GERD cases |
| Smoking history | 2-3 times higher risk | Multiples risk when combined with GERD |
| Family history | 2-4 times higher risk | Close relatives with esophageal cancer |

Red Flags That Need Immediate Attention
- Dysphagia (difficulty swallowing), present in 80% of esophageal cancer cases at diagnosis
- Unexplained weight loss of 10+ pounds in 6 months without diet changes
- Persistent heartburn occurring more than twice weekly for 5+ years
- Food impaction (feeling food stuck in throat or chest) in 30-40% of cases
- Chronic hoarseness or cough lasting over 2 weeks

Prevention and Management
Quitting smoking reduces esophageal cancer risk by 50% within 10 years of cessation. Limiting alcohol to ≤1 drink per day for women and ≤2 for men lowers risk by 25-30%. Losing 5-10% of body weight cuts GERD symptoms by 40% in obese patients (BMI ≥30). Consistent use of Proton Pump Inhibitors (PPIs) for 5+ years lowers cancer risk by 70% in Barrett's esophagus patients.
For high-risk individuals-such as white men over 50 with chronic GERD (5+ years) plus two additional risk factors-endoscopic screening is recommended. The American College of Gastroenterology's 2022 guidelines emphasize this approach to catch precancerous changes before they become cancerous.
Is all GERD dangerous?
No. While chronic GERD increases esophageal cancer risk, most people with GERD do not develop cancer. Only 10-15% of chronic GERD patients develop Barrett's esophagus, and of those, just 0.2-0.5% per year progress to cancer. However, it's important to monitor symptoms and seek medical advice if you have long-term GERD or other risk factors.
What is Barrett's esophagus?
Barrett's esophagus is a condition where the normal lining of the esophagus changes to resemble stomach tissue due to long-term acid exposure from GERD. It's the only known precursor to esophageal adenocarcinoma. While only 0.5-2% of GERD patients develop Barrett's, it significantly increases cancer risk and requires regular monitoring via endoscopy.
How often should I get screened for Barrett's esophagus?
Screening recommendations depend on your risk level. For white men over 50 with chronic GERD (5+ years) and two additional risk factors (like obesity or smoking), the American College of Gastroenterology recommends an initial upper endoscopy. If Barrett's is found, follow-up screenings every 2-5 years are standard. For low-risk individuals, routine screening isn't typically advised.
Can lifestyle changes reduce my risk?
Absolutely. Quitting smoking reduces risk by 50% within 10 years. Losing 5-10% of body weight can cut GERD symptoms by 40% in obese patients. Limiting alcohol intake and avoiding late-night meals also help manage GERD. Consistent PPI use under medical supervision can reduce cancer risk by 70% in Barrett's esophagus patients.
Why is early detection so important?
Esophageal cancer is often diagnosed at advanced stages because early symptoms are mild or dismissed. When caught early (localized stage), the 5-year survival rate jumps to 50-60%, compared to 21% for all stages combined. Endoscopic screening for Barrett's esophagus allows doctors to detect precancerous changes before they become cancerous, significantly improving outcomes.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.