When you’re pregnant and diagnosed with gestational diabetes, the first thing you hear is: food is your medicine. It’s not about cutting out carbs entirely-it’s about choosing the right ones, at the right times, in the right amounts. This isn’t a diet to lose weight. It’s a plan to keep you and your baby healthy, reduce the risk of complications, and avoid insulin if possible. And the good news? Most women can manage it with food alone.
What Your Blood Sugar Numbers Should Be
Your doctor isn’t just giving you random numbers. These targets are based on decades of research showing what’s safest for your baby. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) sets the global standard: fasting blood sugar under 95 mg/dL, one hour after eating under 140 mg/dL, and two hours after eating under 120 mg/dL. If you’re using a continuous glucose monitor (CGM), aim to stay between 70 and 140 mg/dL for most of the day.
Why these numbers? Going over 140 mg/dL after meals means your baby is getting too much sugar. That can lead to excessive growth-babies over 9 pounds are more likely to need a C-section or suffer shoulder injuries during birth. High sugar levels also raise the chance of your baby having low blood sugar right after birth, which can be scary and require extra monitoring. Staying within target cuts those risks by more than half.
Many women think they need to check their sugar after every meal. That’s not always necessary. Most providers recommend checking fasting and one or two hours after your largest meal. If you’re doing well for a week or two, you might reduce to every other day. The goal isn’t perfection-it’s consistency.
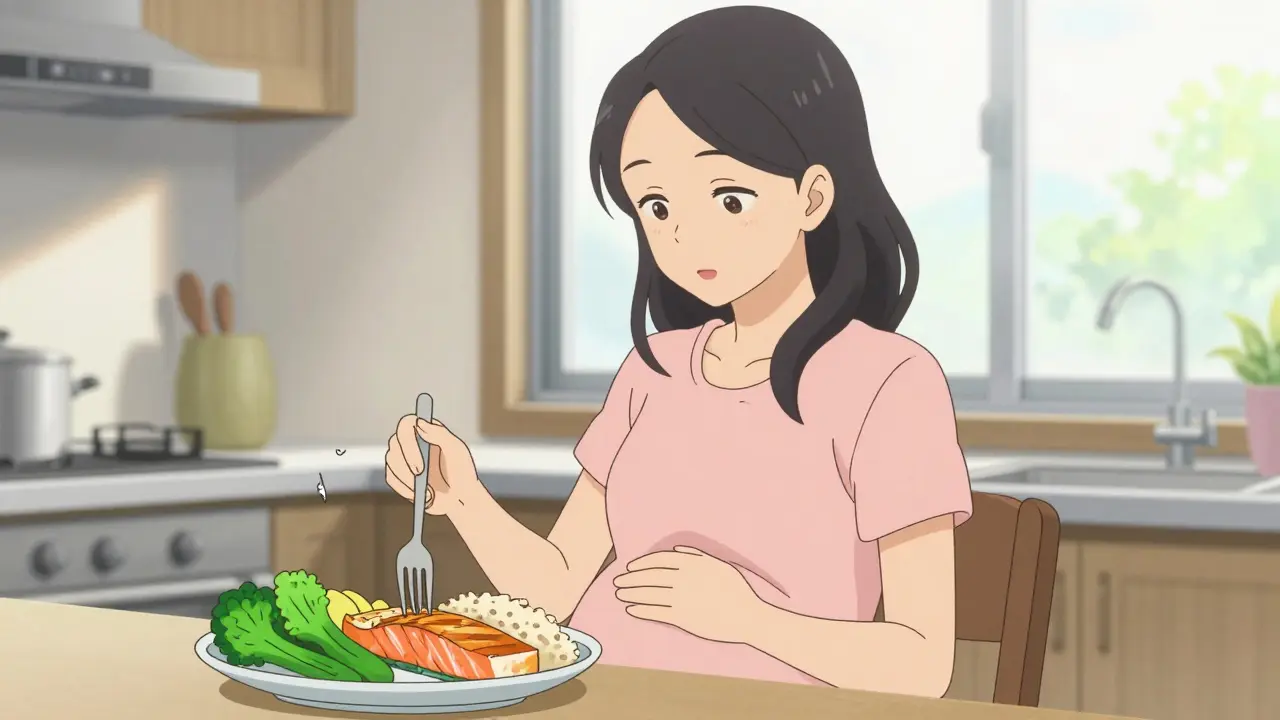
The Plate Method: Simple, Visual, and Effective
Trying to count grams of carbs while nauseous at 7 a.m. is exhausting. That’s why the plate method works so well for so many women. It’s not fancy. It doesn’t require scales or apps. You just divide your plate.
- Half your plate: non-starchy vegetables-broccoli, spinach, peppers, zucchini, cauliflower, salad greens. These are low in carbs and high in fiber, which slows sugar spikes.
- One-quarter: lean protein-chicken, fish, eggs, tofu, lean beef, or legumes. Protein helps you feel full and stabilizes blood sugar.
- One-quarter: carbohydrate sources-brown rice, quinoa, whole wheat bread, oats, sweet potatoes, or fruit. Stick to one serving per meal.
One serving of carbs equals about 15 grams. That’s half a cup of cooked brown rice, one small apple, or one slice of whole grain bread. A tennis ball is a good visual for half a cup of grains. A deck of cards is about the size of 3 ounces of meat.
A 2020 study in the Journal of the Academy of Nutrition and Dietetics found women using the plate method had the same blood sugar control as those counting carbs-but 37% more stuck with it. Why? Because it’s easy. You don’t need to calculate net carbs or memorize charts. You just look at your plate.
Carbohydrate Counting: Precision for Those Who Need It
If you’ve had prediabetes before pregnancy, or if your blood sugar stays high even with the plate method, you might need more precision. That’s where carbohydrate counting comes in.
The American Diabetes Association recommends 45 to 60 grams of net carbs per meal and about 15 grams per snack. Net carbs = total carbs minus fiber. So if a serving of oats has 20 grams of total carbs and 5 grams of fiber, that’s 15 net carbs.
Here’s what a typical day looks like with carb counting:
- Breakfast: 2 scrambled eggs + 1 slice whole grain toast + ½ cup berries = 45g net carbs
- Mid-morning snack: 1 small apple + 1 tablespoon almond butter = 15g net carbs
- Lunch: 3 oz grilled chicken + 1 cup spinach salad + ½ cup quinoa = 45g net carbs
- Afternoon snack: 1 cup Greek yogurt + ¼ cup blueberries = 15g net carbs
- Dinner: 4 oz baked salmon + 1 cup roasted broccoli + ½ cup sweet potato = 45g net carbs
- Evening snack: 1 oz cheese + 1 small pear = 15g net carbs
That’s 240 grams of net carbs a day-spread out so your body doesn’t get overwhelmed. This approach works best for women who are comfortable reading labels or using a food tracking app. But it’s not for everyone. A 2022 survey found 42% of women found carb counting too stressful, especially with morning sickness.

Timing Matters More Than You Think
It’s not just what you eat-it’s when. Your body’s insulin resistance gets worse in the third trimester, and your liver starts pumping out extra glucose overnight. That’s why fasting levels often rise, even if your meals are perfect.
Dr. Loralei Thornburg, a leading expert in pregnancy and blood sugar, says: “Spreading carbs evenly across three meals and three snacks prevents your liver from overproducing sugar.” Skipping meals or going long without eating can make fasting sugar worse.
Here’s what works:
- Don’t go more than 4 to 5 hours without eating.
- Always pair carbs with protein or fat-this slows absorption.
- Try to eat dinner at least 2 hours before bed.
- Keep a bedtime snack with protein and a small amount of carbs-like cheese and a few berries-to help stabilize overnight sugar.
One woman on Reddit, u/Pregnant_and_Worried, said: “I used to skip snacks because I was tired. My fasting sugar shot up to 110. Once I started having cheese and an apple before bed, it dropped to 87. It was that simple.”
What to Eat (and What to Avoid)
Not all carbs are created equal. High-fiber, low-glycemic foods are your friends. Fiber slows digestion, which means sugar enters your bloodstream slowly.
Best choices:
- Whole grains: oats, quinoa, barley, brown rice, whole wheat bread
- Legumes: lentils, chickpeas, black beans (they’re high in fiber and protein)
- Non-starchy vegetables: everything green, broccoli, cauliflower, tomatoes, cucumbers
- Fruits: berries, apples, pears, oranges (limit to one small serving per meal)
- Healthy fats: avocado, olive oil, nuts, seeds
- Protein: eggs, chicken, fish, tofu, Greek yogurt, cottage cheese
Limit or avoid:
- White bread, white rice, pastries, sugary cereals
- Sweetened yogurt, flavored oatmeal, fruit juices
- Processed snacks: chips, cookies, candy
- “Diabetic-friendly” packaged foods-they’re often loaded with sodium and artificial sweeteners
- Large portions of starchy veggies: potatoes, corn, peas (stick to small servings)
And please, don’t fall for the “sugar-free” trap. Many products replace sugar with maltodextrin or dextrose-both raise blood sugar just as fast. Always check the nutrition label for total carbs and fiber.
Real-Life Success Stories
One woman, Maria G., 32, from Ohio, followed her dietitian’s “protein-first” rule: eat protein before carbs at every meal. She’d have a boiled egg or a spoon of cottage cheese before her toast. Her fasting sugar stayed at 87 mg/dL throughout her third trimester. She didn’t need insulin.
A Filipino mom in California shared how she adapted her family’s adobo chicken recipe: she used less soy sauce, added vinegar to lower the glycemic load, and served it with half a cup of brown rice instead of white. “It tasted like home,” she said. “And my sugar stayed normal.”
On the flip side, women who tried extreme low-carb diets (under 1,700 calories a day) often ended up with low iron or folate-risking neural tube defects. One 2022 study found those women had an 18% higher chance of complications. Balance is key.

Tools and Support That Actually Help
You don’t have to do this alone. Here’s what actually works:
- Visual guides: Use a tennis ball to measure half a cup of rice. A deck of cards for meat. Your fist for a cup of veggies.
- Apps: MyFitnessPal or MySugr can help track carbs if you’re comfortable with them. But skip the ones that force you to log every bite-it adds stress.
- Community: The Facebook group “Gestational Diabetes Support” has 147,000 members. People post photos of their plates, ask for recipe swaps, and share blood sugar logs. 89% say it reduced their anxiety.
- Telehealth dietitians: Most insurance now covers virtual nutrition visits. A 2023 Kaiser Permanente study showed women who met with a dietitian twice had 30% better blood sugar control.
And if you’re struggling? That’s normal. A 2021 study found 15% of women with gestational diabetes developed disordered eating patterns because of the pressure to measure everything. If you feel obsessed, anxious, or guilty about food-tell your provider. You deserve support, not shame.
What Happens After Baby Is Born?
Good news: gestational diabetes usually goes away after delivery. But it’s not over. Women who’ve had GDM have a 50% higher risk of developing type 2 diabetes in the next 10 years. That’s why you’ll get a glucose test 6 to 12 weeks after birth.
Keep eating the way you did during pregnancy-whole foods, balanced meals, regular movement. Breastfeeding helps too-it lowers your blood sugar and improves insulin sensitivity. And if you plan to get pregnant again, start with a healthy weight and regular activity. Prevention is easier than treatment.
Can I eat fruit with gestational diabetes?
Yes, but choose wisely. Berries, apples, pears, and oranges are low-glycemic and high in fiber. Stick to one small serving per meal-about 1 cup of berries or one small apple. Avoid fruit juice, dried fruit, and tropical fruits like mango or pineapple in large amounts. Always pair fruit with protein or fat, like a handful of nuts or a spoon of Greek yogurt, to slow sugar absorption.
Do I need to avoid all sugar?
You don’t need to cut out sugar completely, but you do need to avoid added sugars. That means skipping soda, candy, pastries, and sweetened yogurts. Natural sugars in whole fruits and dairy are fine in moderation. The issue isn’t sugar itself-it’s how fast it hits your bloodstream. Pairing carbs with protein, fat, or fiber slows that down.
What if I can’t stick to the plan?
It’s okay. No one is perfect. If you have a meal that spikes your sugar, don’t panic. Just get back on track with your next meal. Focus on consistency, not perfection. If you’re overwhelmed, start with one change-like using the plate method or adding a protein snack at night. Small steps add up. And if you’re feeling emotionally stuck, talk to your doctor or a counselor. Mental health matters just as much as blood sugar.
Is the plate method enough, or do I need to count carbs?
For most women, the plate method is enough. It’s simpler, easier to stick with, and just as effective as carb counting. But if you had prediabetes before pregnancy, or if your blood sugar stays high even with the plate method, your provider might recommend carb counting for tighter control. It’s not about which is better-it’s about what works for you.
Can I still eat my cultural foods?
Absolutely. Dietitians now specialize in culturally adapted meal plans. If you love rice, swap white for brown. If you eat beans daily, keep them-they’re high in fiber. If your traditional dish has sugar or oil, reduce it slightly. Many women have successfully managed GDM while eating Mexican, Indian, Filipino, or Middle Eastern meals. The key is portion control and balancing carbs with protein and veggies.
Will I need insulin?
About 15-20% of women with gestational diabetes end up needing insulin. That doesn’t mean you failed. It just means your body needed extra help. Insulin is safe during pregnancy and doesn’t cross the placenta. Many women who start insulin later in pregnancy still have healthy babies. The goal isn’t to avoid insulin-it’s to keep your baby safe. If your provider recommends it, it’s a tool, not a punishment.
What to Do Next
Start today. Grab a plate. Fill half with veggies. Add a palm-sized protein. Top it with a small portion of whole grains or fruit. Drink water. Walk after meals. Check your sugar as advised. Talk to your provider if something feels off.
You’re not just eating for yourself. You’re building a foundation for your baby’s health-and your own. This isn’t a diet you’ll forget after birth. It’s the start of a lifelong habit that protects you from type 2 diabetes, heart disease, and other long-term risks. And the best part? You’re already doing it right by seeking the information. That’s half the battle won.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.