Every year, millions of people take more than one medication. Some take pills for blood pressure, others for cholesterol, diabetes, or pain. Add in vitamins, herbal supplements, or even over-the-counter painkillers, and the mix gets complicated fast. What seems like a harmless combo-like ibuprofen with warfarin or St. John’s wort with antidepressants-can lead to serious side effects, hospital visits, or worse. That’s where drug interaction checkers come in. These tools don’t guess. They scan your meds and tell you what could go wrong.
What Is a Drug Interaction Checker?
A drug interaction checker is a digital tool that looks at the medicines you’re taking and flags dangerous combinations. It doesn’t just say “this might interact.” It tells you how serious it is, what symptoms to watch for, and sometimes even what to do instead. These tools are used by doctors, pharmacists, and patients alike. Some live inside hospital systems like Epic or Cerner. Others are free apps on your phone, like Medisafe or Epocrates.
They work by matching your drugs against a database of known interactions. These databases are built from decades of clinical studies, case reports, and real-world data. For example, if you enter lisinopril and potassium supplements, the checker will show you a red alert: combining them can raise your potassium to dangerous levels, risking heart rhythm problems. It’s not theory-it’s based on data from thousands of patients.
Why You Need One (Even If You’re Healthy)
You might think, “I only take two pills. What’s the risk?” But here’s the thing: most people don’t realize how many substances they’re mixing. A 2022 CDC study found that 44% of adults over 65 take five or more medications daily. That’s not rare-it’s normal. And it’s not just prescriptions. Many take fish oil, magnesium, melatonin, or turmeric supplements. Some of these interact with blood thinners, antidepressants, or blood pressure meds.
One woman in Perth, 72, was taking atorvastatin for cholesterol and a common herbal supplement called red yeast rice. She felt fine-until she had muscle pain so bad she couldn’t walk. Her pharmacist ran her meds through a checker and found the combo increased her risk of rhabdomyolysis, a dangerous muscle breakdown. The supplement was pulled, and her symptoms cleared in weeks. That’s the power of a simple check.
Even if you’re young and healthy, you might be on antibiotics, birth control, or painkillers that interact with other meds you didn’t even think of as “medicine.”
Step-by-Step: How to Use a Drug Interaction Checker
Using a drug interaction checker is simple-but only if you do it right. Here’s how:
- Make a complete list of everything you take. Don’t forget: prescription drugs, over-the-counter pills (like antacids or sleep aids), vitamins, minerals, herbal teas, and supplements. Write down the exact names and doses. For example: “ibuprofen 400 mg,” not just “painkiller.”
- Choose your tool. If you’re a patient, use a consumer app like Medisafe (iOS/Android) or Epocrates. If you’re a healthcare provider, use Lexi-Interact, Micromedex, or DrugBank. All of them work similarly.
- Enter each drug one at a time. Type the name into the search bar. Don’t guess. If you type “aspirin,” the tool might show you 10 versions: enteric-coated, low-dose, buffered. Pick the one that matches what you’re taking. This step matters-wrong selections cause false alerts.
- Review the results. Most tools color-code the results: red = dangerous, avoid; orange = caution, monitor; yellow = minor, note it; green = safe. Click on any flagged interaction to see what happens. For example: “Warfarin + NSAIDs = increased bleeding risk. Symptoms: unusual bruising, nosebleeds, dark stools.”
- Don’t ignore the details. Some interactions only happen with certain doses, routes (oral vs. injection), or timing. A checker might say “avoid with grapefruit juice” or “take 2 hours apart.” Read the full explanation.
- Share the results with your doctor or pharmacist. Don’t stop or change your meds based on a checker alone. Use it as a conversation starter. Say: “I saw this alert. Should I be worried?”
Top Tools Compared: What Works Best?
Not all checkers are equal. Here’s how the main ones stack up:
| Tool | Best For | Accuracy | Ease of Use | Cost |
|---|---|---|---|---|
| Medisafe (App) | Patients, daily users | Good | Very easy | Free |
| Lexi-Interact | Pharmacists, hospitals | Excellent | Complex | $1,500+/year (institutional) |
| Epocrates | Doctors, quick checks | High | Very fast | Free (basic), $99/year (premium) |
| DrugBank API | Developers, tech integrations | Excellent | Requires coding | Subscription-based |
| University of Liverpool DDI Checker | COVID-19 meds only | Excellent for its scope | Simple | Free |
For most people, Medisafe or Epocrates are the best starting points. They’re free, fast, and work on your phone. If you’re a clinician, Lexi-Interact or Micromedex are the gold standard-they catch more subtle interactions and include food, alcohol, and supplement data.
Common Mistakes (And How to Avoid Them)
Even experienced users mess up. Here are the top errors:
- Using generic names. Typing “ibuprofen” instead of “ibuprofen 200 mg” can miss interactions tied to dose or formulation.
- Forgetting supplements. People skip these, but St. John’s wort, ginkgo, garlic, and vitamin E all interact with common meds.
- Ignoring severity levels. A yellow alert isn’t “no problem.” It means “watch for X symptom.”
- Trusting one tool only. A 2016 NIH study found that using two checkers together caught 30% more dangerous interactions than using one.
- Not checking after a change. If your doctor adds or removes a drug, re-run the checker. Interactions change with every new pill.
Pro tip: Keep your list updated in your phone notes. Update it every time you get a new prescription or refill.
What the Experts Say
Dr. David Bates from Brigham and Women’s Hospital says DDI checkers prevent about 1.5 million adverse events in U.S. hospitals each year. But he also warns: “They miss 15-40% of real risks.” Why? Because they don’t know your full health picture. Your liver function, age, kidney health, or genetics can change how a drug behaves.
Pharmacists at Johns Hopkins reduced false alerts by 70% by customizing their system to only flag high-risk combos for their patients. That’s the key: tools are smart, but humans are smarter. Use them as assistants-not replacements.
And don’t fall for alert fatigue. One study found that doctors ignored nearly half of all interaction alerts because they were too noisy. That’s why you need to pick a tool that lets you filter alerts by severity and relevance.
What’s Next for Drug Interaction Checkers?
The next wave is personalization. Mayo Clinic is testing systems that use your DNA to predict how you’ll react to certain drugs. Imagine a checker that says, “Based on your genes, this statin could cause muscle damage in you-try an alternative.”
Also, real-world data is now being fed into these tools. The FDA’s Sentinel Initiative tracks millions of patient records to spot patterns no lab study could catch. By 2025, most major checkers will include this live data.
For now, stick with what works: a reliable tool, a complete list, and a conversation with your pharmacist. Don’t wait for a crisis to check your meds.
Can I trust free drug interaction checkers on my phone?
Yes, if they’re from reputable sources like Medisafe, Epocrates, or DrugBank. These tools use the same databases as hospital systems. But don’t rely on random apps from unknown developers. Stick to ones backed by pharmacists or major health institutions.
Do drug interaction checkers include supplements?
The best ones do. Lexi-Interact, Micromedex, and DrugBank include hundreds of supplements. Consumer apps like Medisafe also cover common ones like melatonin, magnesium, and fish oil. But some cheaper or older tools still ignore supplements. Always check the tool’s documentation or help section to confirm.
What if the checker says there’s no interaction, but I feel weird?
Trust your body. DDI checkers aren’t perfect. They’re based on known data, but new interactions are still being discovered. If you feel dizzy, nauseous, or have unusual symptoms after starting a new med, talk to your doctor-even if the checker says it’s safe. Sometimes, it’s not the combo-it’s how your body is reacting.
Do I need to check interactions every time I refill a prescription?
Yes. Your meds change. Maybe you started a new one, stopped another, or your dose changed. Even a small change can create a new risk. Make it a habit: check every time you get a new prescription or refill a bottle. It takes less than 2 minutes.
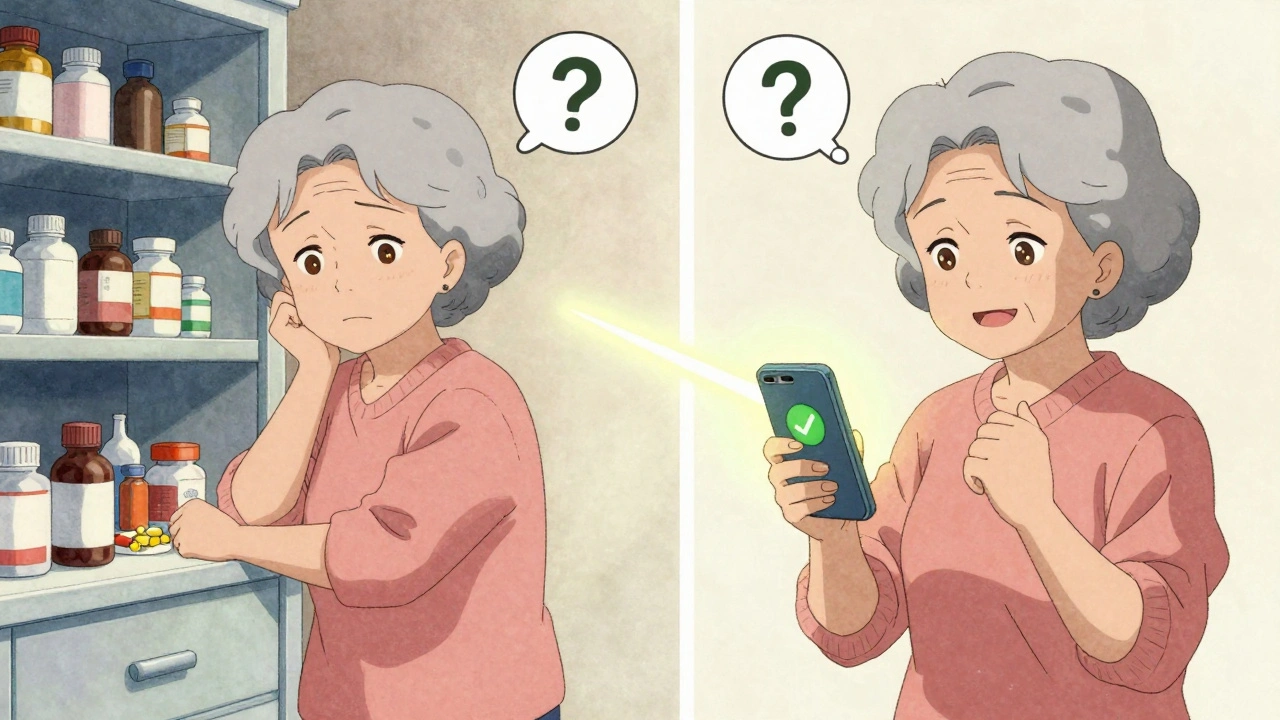
Can I use a drug interaction checker for my elderly parent?
Absolutely. Older adults are at highest risk because they often take 5-10 medications. Use Medisafe or Epocrates together with them. Sit down, enter all their pills-including creams, patches, and inhalers-and review the results out loud. This is one of the best ways to prevent a hospital trip.
Final Step: Make It a Habit
Drug interaction checkers aren’t magic. They’re tools. And like any tool, they’re only as good as the person using them. The goal isn’t to scare you-it’s to give you control. You’re not just taking pills. You’re managing your health. And with a few minutes every few weeks, you can avoid a lot of pain, cost, and risk.
Start today. Open your phone. Open your medicine cabinet. Write down every pill, patch, and powder. Then run it through a checker. You might not find anything. Or you might find the one thing that’s keeping you from feeling your best.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.