When you fill a prescription for a brand-name drug like Protonix or Yasmin, you might be surprised to find a pill that looks different but works exactly the same. That’s an authorized generic-a drug made by the original brand company but sold without the brand name. For insurers, these drugs are a quiet win: same effectiveness as the brand, same safety profile, but priced like a regular generic. Yet, getting them covered isn’t always straightforward. Many patients and even pharmacists don’t realize they’re getting an authorized generic, and insurers often treat them inconsistently. Understanding how formulary placement works for these drugs can mean the difference between paying $10 or $50 for the same medication.
What Exactly Is an Authorized Generic?
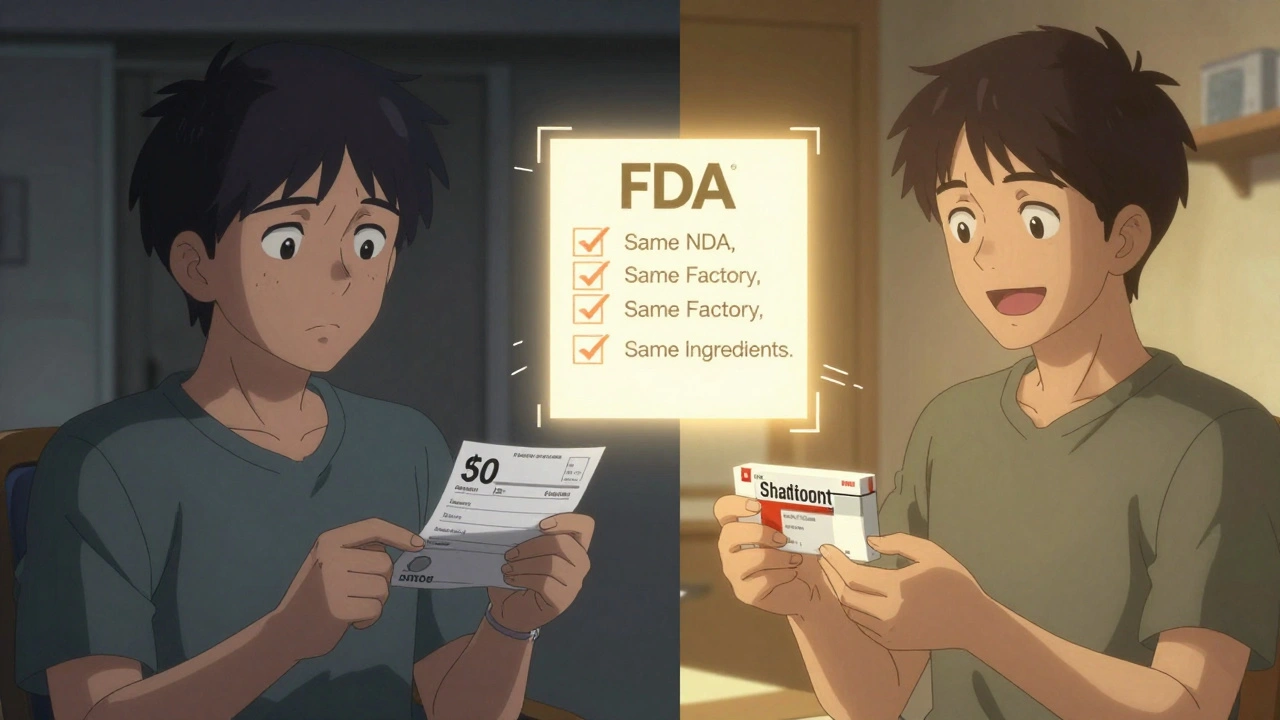
An authorized generic isn’t just another generic. It’s the exact same drug as the brand-name version, made by the same company, using the same factory, same ingredients, same process. The only difference? No brand name on the label. Think of it like buying a Coca-Cola bottle with the logo removed-it’s still Coca-Cola. The FDA defines it as a drug approved under the original New Drug Application (NDA), meaning it skips the usual generic approval process. That’s why it’s considered therapeutically identical, not just bioequivalent.
Unlike traditional generics, which must prove they work the same through costly bioequivalence studies, authorized generics don’t need to. They’re already approved under the brand’s NDA. This lets them hit the market faster-sometimes even before the first traditional generic arrives. As of 2023, the FDA listed 147 active authorized generics, including drugs for high blood pressure, thyroid conditions, and birth control. But here’s the catch: only about 15-20% of brand-name drugs have an authorized generic version. That means most patients still face the choice between expensive brands and uncertain generics.
Why Insurers Care About Formulary Placement
Insurance plans organize drugs into tiers to control costs. Tier 1 is usually the cheapest-often generic drugs. Tier 3 or 4 is for brand-name drugs with higher copays. Authorized generics should logically sit in Tier 1 or 2, right? In theory, yes. In practice, it’s messy.
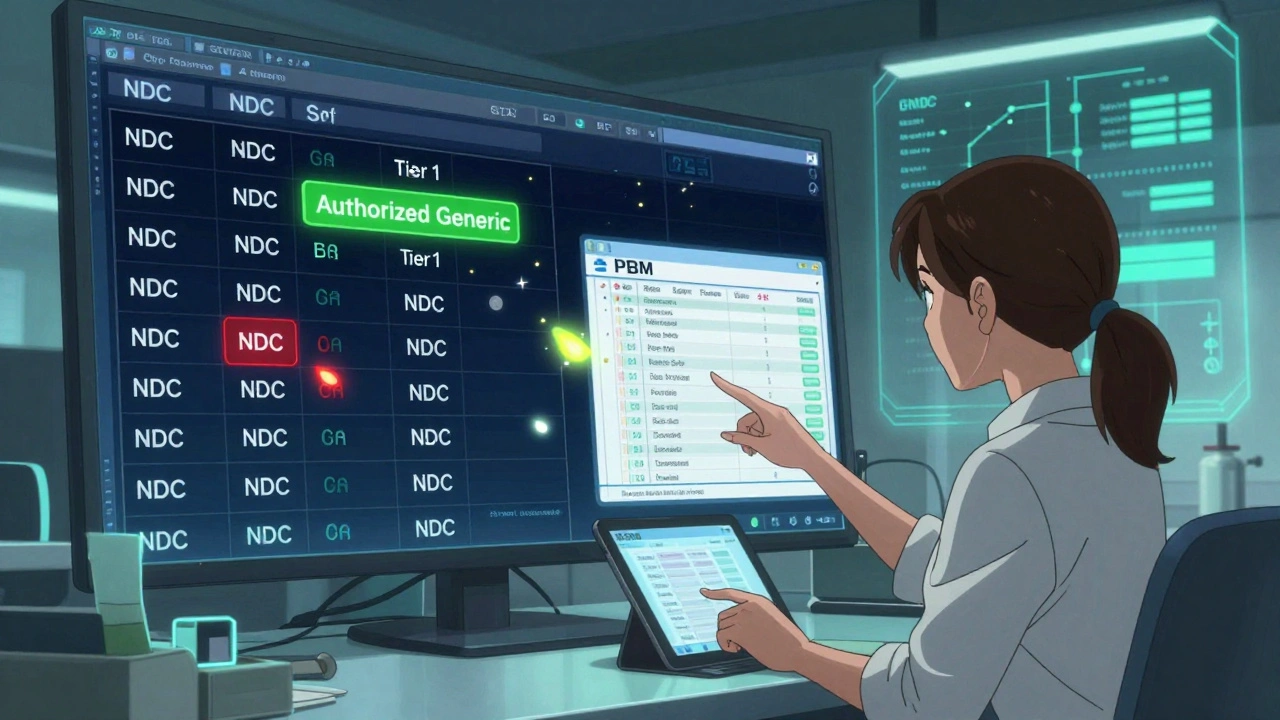
A 2022 study of 1,247 Medicare Part D plans found that 87% placed authorized generics in the same tier as traditional generics. That’s good news. But 12% still treated them like brand-name drugs, forcing patients to pay more. Why? Because many pharmacy benefit managers (PBMs) don’t have clear systems to identify them. Authorized generics aren’t listed in the FDA’s Orange Book, which most pharmacy systems use to classify drugs. Without proper coding, a system might flag them as unknown or even reject the claim.
For insurers, placing authorized generics correctly means saving money without risking patient outcomes. A patient on Synthroid with an allergy to a dye in the brand version can switch to the authorized generic safely-and save $40 a month. That’s not just a win for the patient. It’s a win for the plan. Studies show that plans with clear policies on authorized generics cut per-member-per-month costs by 7.3%. That’s real savings.
How Authorized Generics Compare to Traditional Generics
It’s easy to assume all generics are the same. But they’re not. Here’s how authorized generics stack up:
| Feature | Authorized Generic | Traditional Generic |
|---|---|---|
| Manufacturer | Same as brand-name drug | Separate company |
| Approval Path | Under brand’s NDA | Abbreviated New Drug Application (ANDA) |
| Ingredients | Identical to brand | Same active ingredient, may differ in fillers |
| Market Entry Timing | Can launch immediately after brand patent expires | Subject to 180-day exclusivity for first filer |
| Formulary Tier | Usually Tier 1 or 2 | Usually Tier 1 or 2 |
| Cost to Patient | Same as traditional generic | Same as authorized generic |
The biggest practical difference? Allergies. Traditional generics sometimes use different inactive ingredients-dyes, preservatives, fillers-that can trigger reactions in sensitive patients. Authorized generics avoid this because they’re chemically identical. For someone with severe allergies or conditions like epilepsy, where even tiny variations matter, this isn’t just a convenience-it’s a safety issue.
Real Patient Experiences
On Reddit’s r/Pharmacy community, users shared stories of how authorized generics saved them money-and sometimes their health. One person wrote: "My insurance denied my brand Synthroid because it was too expensive. The authorized generic? Approved with a $10 copay. My thyroid levels stayed perfect. No side effects."
But it’s not always smooth. A 2022 GoodRx survey found that 34% of patients didn’t know they’d been switched to an authorized generic. Some were shocked when their pharmacy handed them a different-looking pill. Others got denied coverage because their plan’s system didn’t recognize the NDC code. One user reported being charged the brand copay for weeks before the pharmacy updated their records.
Pharmacies are getting better. Express Scripts reported that 89% of authorized generic claims were approved on the first try in 2023. That’s close to the 92% approval rate for traditional generics. But the gap still exists. It’s not a system failure-it’s a data gap. Many pharmacy systems still rely on outdated databases that don’t flag authorized generics properly.
How Insurers and PBMs Are Adapting
Major pharmacy benefit managers are starting to act. OptumRx rolled out an "Authorized Generic First" policy in January 2023 for 47 high-cost medications. That means if an authorized generic exists, it’s the default covered option unless the doctor specifically requests the brand. Express Scripts added special flags to their formulary system in late 2022 to make identification easier.
CVS Caremark says it takes 30 to 45 days from a product’s launch to fully integrate an authorized generic into their formulary. That’s fast compared to the old way, where it could take months. But it’s still not automatic. It requires manual updates, staff training, and system checks. Walgreens reported a 12% error rate in early processing-claims getting rejected or misclassified-until they built a verification tool to cross-check the FDA’s authorized generic list.
The key? Using the right tools. Prime Therapeutics’ AG Tracker, as of mid-2023, covered 98% of available authorized generics. That’s the kind of system insurers need. Without it, they’re flying blind.
The Bigger Picture: Market Trends and Policy Shifts
The U.S. authorized generic market hit $4.7 billion in 2022. That’s just 3.2% of the total generic drug market, but it’s growing fast-at 8.4% per year through 2027. Why? Because drugmakers are using them as a tool to hold onto market share. When a patent expires, instead of letting a cheaper generic take over, they launch their own authorized version. It keeps revenue flowing and delays competition.
That’s sparked criticism. Dr. Peter Bach from Memorial Sloan Kettering found that in 22% of cases, authorized generics slowed down true generic competition. The FTC flagged this as a potential anti-competitive practice in 2022. But for patients and insurers, the immediate benefit is clear: lower prices without switching risks.
The Inflation Reduction Act of 2022 is pushing things further. Medicare Part D is expected to increase authorized generic coverage by 15-20% by 2025 as part of efforts to cap out-of-pocket costs. Large employers are also taking notice. According to the Kaiser Family Foundation, 68% plan to treat authorized generics differently than traditional generics in 2024-either by lowering copays or making them preferred options.
What Patients Should Do
If you’re on a brand-name drug and your copay is high, ask your pharmacist: "Is there an authorized generic for this?" Don’t assume it’s not available. Check the FDA’s official list. If one exists, ask your doctor to write the prescription for the generic version. Some doctors don’t know these exist.
If your insurance denies coverage or charges you a brand copay, call them. Ask: "Why is this being treated as a brand drug?" Show them the FDA’s authorized generic list. Most plans have policies to cover them-just not everyone knows it.
And if you’re switching from a brand to an authorized generic, keep an eye out. If you feel different-new side effects, worse control of your condition-talk to your doctor. It’s rare, but inactive ingredients can still vary slightly between manufacturers, even with authorized generics. Your health isn’t worth guessing.
Final Thoughts
Authorized generics are one of the best-kept secrets in drug pricing. They offer brand-level reliability at generic prices. But for patients to benefit, insurers need to get them right on formularies. The technology exists. The data is available. The savings are real. The missing piece? Awareness.
It’s not about choosing between brand and generic anymore. It’s about choosing between brand, generic, and the smart middle ground: the authorized generic. If your plan doesn’t cover it properly, speak up. Your wallet-and your health-will thank you.
Are authorized generics the same as brand-name drugs?
Yes. Authorized generics contain the exact same active and inactive ingredients as the brand-name drug, are made in the same facility, and follow the same manufacturing process. The only difference is the packaging and labeling-they don’t carry the brand name. The FDA considers them therapeutically identical.
Why are authorized generics cheaper than brand-name drugs?
They’re cheaper because they don’t carry the marketing, advertising, and research costs associated with brand-name drugs. Since they’re produced by the original manufacturer under the same NDA, they avoid the high costs of launching a new product. Insurers and pharmacies negotiate lower prices, passing the savings to patients.
Can I ask my doctor to prescribe an authorized generic?
Absolutely. You can ask your doctor to prescribe the generic version by name or by NDC code. Many doctors aren’t aware authorized generics exist, so bringing it up helps. If the brand is expensive and an authorized generic is available, it’s a safe and cost-effective switch.
Why does my insurance sometimes deny coverage for an authorized generic?
It’s usually a system error. Authorized generics aren’t listed in the FDA’s Orange Book, so many pharmacy databases don’t recognize them automatically. The NDC code may be missing or misclassified. Call your insurer and ask them to check if the drug is on their authorized generic list. Most plans will correct it once they verify.
Are authorized generics available for all medications?
No. Only about 15-20% of brand-name drugs have an authorized generic version. They’re most common in cardiovascular, endocrine, and psychiatric drugs, and rare in oncology and rare disease treatments. Always check the FDA’s official list to see if one exists for your medication.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.