When you’re stuck in a fog that won’t lift-no matter how hard you try to shake it-you’re not weak. You’re not lazy. You might be dealing with major depressive disorder (MDD). It’s not just feeling sad. It’s losing interest in everything you once loved, sleeping too much or too little, feeling worthless, or even having thoughts that life isn’t worth living. And if you’ve been feeling this way for two weeks or more, it’s time to look at real, proven treatment options-not just hoping it gets better on its own.
What Major Depressive Disorder Really Looks Like
Major Depressive Disorder isn’t a phase. It’s a medical condition, recognized since 1980 in the DSM, and it affects about 15.5% of U.S. adults every year. That’s roughly one in six people. Symptoms don’t come and go with the weather. They stick around. You might cry for no reason, feel exhausted even after sleeping, or struggle to get out of bed. Some people lose weight. Others gain it. Some can’t concentrate enough to read a text message. And for many, there’s no clear trigger-no breakup, no job loss, no death. It just shows up. The brain chemistry involved is real. Neurotransmitters like serotonin and norepinephrine aren’t working the way they should. But MDD isn’t just about chemicals. It’s also about how you think, how you relate to others, and how your environment shapes your mood. That’s why the best treatments don’t just target one thing-they target multiple parts of the problem.Psychotherapy: Talking Your Way Out of the Dark
If you’ve ever thought therapy is just “talking about your feelings,” you’re missing the point. Evidence-based psychotherapy for depression is structured, time-limited, and backed by decades of research. It’s not vague advice. It’s skill-building. The most studied and recommended form is Cognitive Behavioral Therapy (CBT). CBT doesn’t tell you to “think positive.” It teaches you to spot the automatic, distorted thoughts that keep you stuck. Like: “I failed at this task, so I’m a failure.” CBT helps you test that thought. Is it true? Is it helpful? What’s another way to see it? Studies show CBT reduces symptoms by more than 50% in many patients within 12 to 20 sessions. Another powerful option is Behavioral Activation. This is CBT’s simpler cousin. Instead of digging into thoughts, it focuses on action. When you’re depressed, you stop doing things that used to bring joy. You isolate. You sleep. You scroll. Behavioral activation asks you to schedule one small, pleasant activity each day-even if you don’t feel like it. Walk around the block. Call a friend. Sit outside with coffee. Over time, doing these things rewires your brain to associate activity with reward again. Then there’s Interpersonal Therapy (IPT). This one doesn’t focus on your thoughts. It focuses on your relationships. Maybe you’re stuck in a toxic friendship. Maybe you’re grieving someone you lost. Maybe you’re feeling disconnected from your partner. IPT helps you fix those holes in your social support system, which often plays a huge role in depression. For people who can’t get to a therapist’s office-because of location, mobility, or stigma-Computerized CBT (CCBT) is a real alternative. Apps and online programs deliver CBT modules through videos, quizzes, and journal prompts. They’re not perfect. You don’t get the emotional connection of a real therapist. But for mild to moderate depression, they work. And they’re getting better.Antidepressants: What Actually Works
Medication isn’t a magic pill. But for many people, it’s the missing piece. The first-line drugs today are second-generation antidepressants. That means they’re safer and have fewer side effects than older ones like tricyclics. The most common are SSRIs (Selective Serotonin Reuptake Inhibitors): escitalopram, sertraline, fluoxetine, paroxetine. They’re usually the first choice because they’re well-tolerated. But they’re not all the same. Some cause more nausea. Others make you sleepy. Some delay sexual function. It often takes trying one or two to find the right fit. If SSRIs don’t cut it, doctors often turn to SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) like venlafaxine or duloxetine. These affect two neurotransmitters instead of one. They can be more effective for severe depression, especially when fatigue and lack of energy are big problems. Some older drugs still have a place. Mirtazapine helps with sleep and appetite loss. Amitriptyline is powerful but comes with more side effects-dry mouth, dizziness, weight gain. It’s usually reserved for cases where newer drugs failed. Here’s what to expect: You won’t feel better in a week. Most people notice small improvements after two to four weeks. Full effects take eight to twelve weeks. And yes-some people feel worse before they feel better. That’s normal. It’s not a sign the drug isn’t working. It’s your brain adjusting. Side effects are real. Nausea, weight gain, sexual dysfunction, insomnia. But they often fade after a few weeks. If they don’t, your doctor can adjust the dose or switch you to another medication. Don’t quit cold turkey. That can cause withdrawal symptoms like dizziness, brain zaps, or flu-like feelings.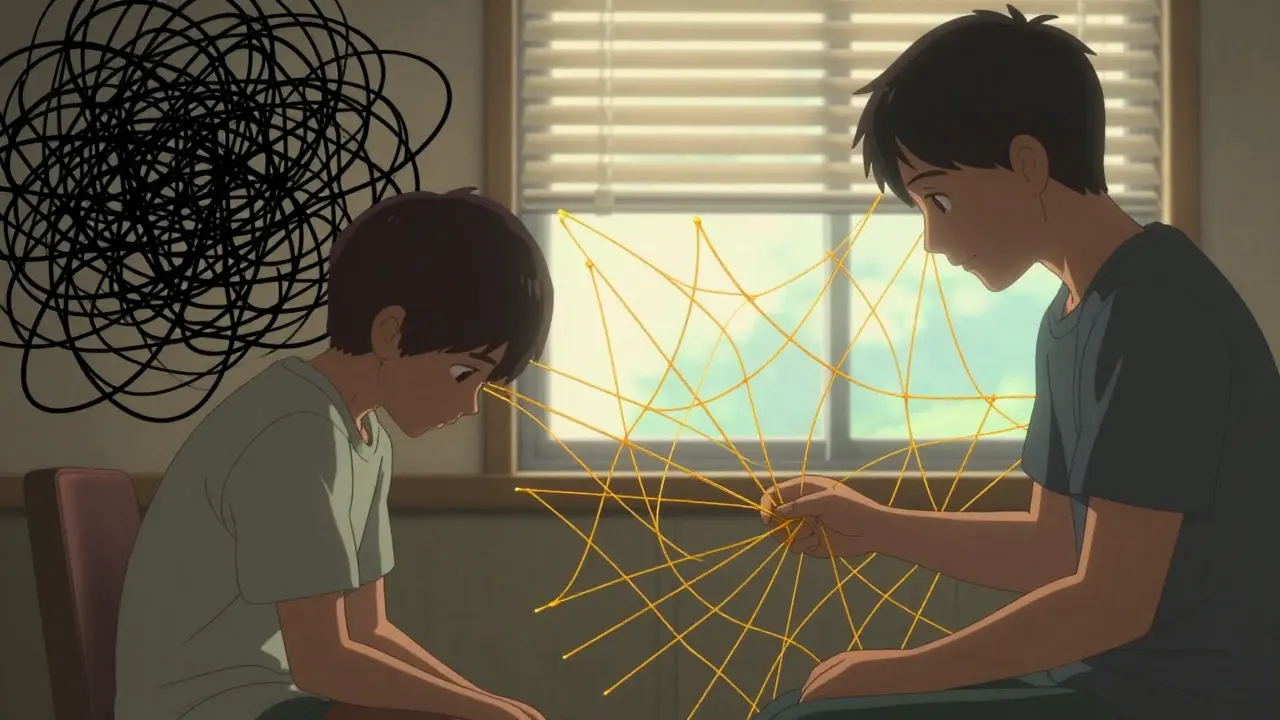
Combination Therapy: The Gold Standard
Here’s the most important thing to know: Combining antidepressants with psychotherapy works better than either alone-especially for moderate to severe depression. A 2025 review in Nature found that while medication and therapy are equally effective on their own, together they boost recovery rates by 20-30%. Why? Because medication helps stabilize your mood enough to actually do the work in therapy. Therapy gives you tools to stay well after the medication stops. Think of it like this: Antidepressants lower the water level in the flood. Therapy teaches you how to build a dam. For someone with a PHQ-9 score of 16 or higher (that’s moderate to severe depression), guidelines from NICE and AAFP strongly recommend starting with both. For mild depression, therapy alone might be enough. For severe cases, skipping therapy means missing out on long-term protection against relapse.What Doesn’t Work (And Why)
Not every option is right for everyone. CBT doesn’t work if you can’t reflect on your thoughts. People with severe cognitive impairment, dementia, or very low motivation might struggle to engage. That’s where medication or behavioral activation becomes more useful. CCBT isn’t for everyone. It needs digital literacy and self-discipline. If you’re too overwhelmed to open an app, it won’t help. And if you’re in crisis, you need a human, not a screen. Antidepressants aren’t for everyone either. If you’re pregnant, breastfeeding, or have certain heart conditions, some meds are risky. Some people simply can’t tolerate side effects. That’s why alternatives like Electroconvulsive Therapy (ECT) exist. It’s not what you see in movies. It’s done under anesthesia. A tiny electric current triggers a brief, controlled seizure. It’s the most effective treatment for treatment-resistant depression. And yes-it works fast. Often in just a few sessions.
Access, Cost, and Real-Life Barriers
Knowing what works is one thing. Getting it is another. In many places, waiting lists for therapy are months long. Rural areas have fewer therapists. Insurance doesn’t always cover enough sessions. And therapy can cost $100-$200 per session without coverage. Telehealth has helped. Many therapists now offer video sessions. CCBT programs are often covered by insurance. Some employers offer free counseling through EAPs (Employee Assistance Programs). And in the U.S., the 988 Suicide & Crisis Lifeline is free, 24/7. Cost shouldn’t be a barrier to care. If you’re struggling, ask your doctor about sliding-scale clinics, community mental health centers, or university training programs where therapy is provided by supervised students at low cost.What Comes Next?
Treatment isn’t a one-size-fits-all fix. It’s a process. You might start with therapy. Then add medication. Then switch meds. Then try a different therapist. That’s normal. The goal isn’t to “get over it.” It’s to build a life where depression doesn’t control you. That means learning coping skills, rebuilding relationships, and finding meaning again-even if it’s small. If you’re reading this and you’re in pain, know this: You’re not broken. You’re not alone. And help exists. Not magic. Not miracles. But real, science-backed tools that have worked for millions. Start by talking to your doctor. Or call a helpline. Or text a friend. Don’t wait for the fog to lift on its own. It won’t. But with the right support, you can learn to walk through it.Can antidepressants cure depression permanently?
No. Antidepressants help manage symptoms, but they don’t fix the underlying causes like negative thought patterns or relationship stress. For long-term recovery, combining medication with psychotherapy gives you tools to stay well after stopping the pills. Many people take antidepressants for 6-12 months after feeling better to prevent relapse.
How long does therapy take to work for depression?
Most people start noticing small improvements in 4-8 weeks of regular therapy. Full benefits usually take 12-20 weekly sessions. Behavioral activation can show results faster-sometimes within 2-3 weeks-because it focuses on action, not just talk. Consistency matters more than speed.
Are SSRIs addictive?
No. SSRIs are not addictive like alcohol, opioids, or benzodiazepines. You won’t crave them or get high from them. But your body can become used to them. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or brain zaps. Always taper off under a doctor’s supervision.
What if therapy doesn’t help me?
It doesn’t mean you failed. Some people need a different type of therapy, a different therapist, or a combination of approaches. If CBT isn’t working, try IPT or behavioral activation. If therapy alone isn’t enough, add medication. If that still doesn’t help, ECT or newer options like ketamine therapy (under strict supervision) may be options. Persistence matters more than perfection.
Can I use apps instead of a therapist?
Apps like Woebot, Moodfit, or CBT-i Coach can help with mild depression or as a supplement to therapy. But they’re not a replacement for human connection. If you’re having thoughts of self-harm, severe hopelessness, or can’t function daily, you need a licensed professional. Apps are tools-not lifelines.
Do antidepressants change your personality?
No. They don’t make you happy or turn you into someone else. What they do is reduce the overwhelming weight of depression so you can feel like yourself again. Some people report feeling emotionally numb at first-that’s a side effect, not the goal. If that happens, talk to your doctor. There are other options.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.