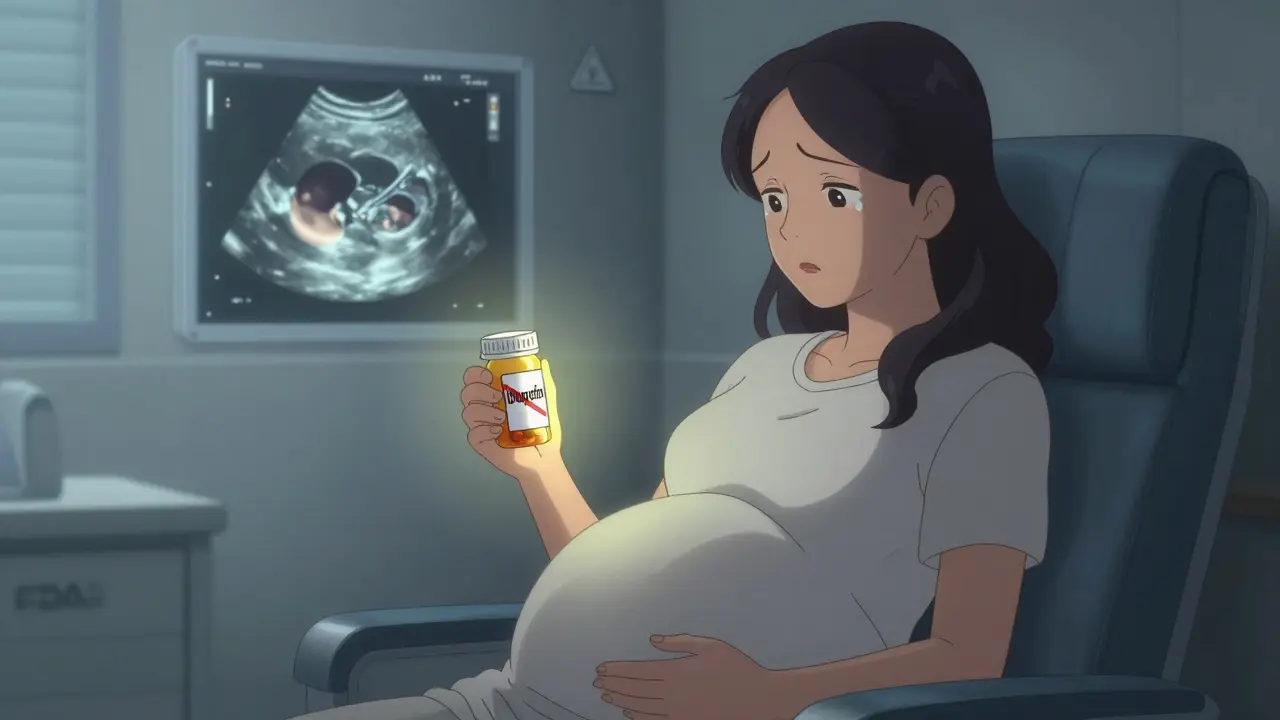
When you're pregnant, every pill, drop, or supplement feels like a decision with two lives on the line. You want to feel better - whether it's a headache, a stuffy nose, or heartburn - but you're terrified of hurting your baby. The truth is, medications to avoid during pregnancy aren't just old wives' tales. Some are backed by decades of research, FDA warnings, and real cases of birth defects. And others? They’re still being studied - with new data changing what we thought we knew.
NSAIDs: More Dangerous Than You Think
Ibuprofen, naproxen, aspirin - these are the go-to pain relievers for millions. But after 20 weeks of pregnancy, they’re no longer safe. The FDA issued a clear warning in October 2020: NSAIDs can cause fetal kidney problems, leading to dangerously low amniotic fluid (oligohydramnios). This isn’t a rare side effect. Studies show a 1.5 to 2 times higher risk when taken after 20 weeks. In some cases, it leads to underdeveloped lungs or even stillbirth. Even low-dose aspirin, once commonly prescribed for preeclampsia prevention, needs careful monitoring. Only doses between 60 and 150 mg daily are considered safe under medical supervision. Anything higher? Skip it. If you’re taking an NSAID for a chronic condition like arthritis, talk to your provider now. There are safer options, and delaying the switch can put your baby at risk.Acetaminophen: The New Controversy
For years, acetaminophen (Tylenol) was the gold standard for pain and fever during pregnancy. But in September 2025, the FDA issued a Notice to Physicians that changed everything. New data from a 95,000-person study published in JAMA Pediatrics showed a 28.6% higher risk of ADHD and a 20.4% higher risk of autism spectrum disorder in children whose mothers took acetaminophen for long periods - especially if used throughout pregnancy. This doesn’t mean you can’t use it. The FDA isn’t saying to stop completely. It’s saying: use the lowest dose for the shortest time possible. If you have a fever of 102°F or higher, the risk from untreated hyperthermia - which can cause neural tube defects - is 8.2 times greater than any potential risk from acetaminophen. So treat the fever. But don’t take Tylenol every day for a mild headache unless you absolutely need to. ACOG still lists acetaminophen as the preferred option, but their 2022 guidelines don’t reflect this new data. The CDC now advises pregnant women to “consider avoiding” it as a precaution. It’s a gray area - and that’s why you need to talk to your provider, not just rely on what you read online.Antibiotics That Can Harm Your Baby
Not all antibiotics are created equal. Tetracyclines - including doxycycline - are a hard no. They bind to developing bones and teeth, causing permanent gray or brown discoloration and weakened enamel. Even a single course can have lifelong effects. Fluoroquinolones like ciprofloxacin (Cipro) and levofloxacin (Levaquin) are linked to a 1.9 times higher risk of musculoskeletal problems in children, including tendon damage and joint issues. These drugs are often prescribed for UTIs or sinus infections - common in pregnancy - but they’re not worth the risk. Safe alternatives like amoxicillin or cephalexin are just as effective and have been studied in thousands of pregnancies with no increased birth defect rates.High Blood Pressure Medications: Act Fast
If you’re on ACE inhibitors (lisinopril, enalapril) or ARBs (valsartan, losartan) and find out you’re pregnant, stop them immediately. These drugs can cause catastrophic harm to the developing fetus: kidney failure, low amniotic fluid, skull underdevelopment, and even death. The risk is so high - 30% to 50% - that doctors recommend switching before conception if you have chronic hypertension. Safe alternatives include methyldopa, labetalol, and nifedipine. These have been used safely in pregnancy for decades. If you’re planning to get pregnant and take blood pressure meds, talk to your doctor now. Don’t wait until you miss your period.
Acne and Seizure Meds: High-Risk, High-Stakes
Isotretinoin (Accutane) is one of the most dangerous drugs in pregnancy. It causes severe birth defects in more than 25% of exposed pregnancies - including missing ears, heart defects, and brain malformations. The FDA’s iPLEDGE program requires strict controls for this drug, but women still get pregnant while taking it. If you’re on isotretinoin and want to conceive, wait at least one month after stopping - but many experts recommend three to six months. Valproic acid (Depakote), used for epilepsy and bipolar disorder, carries a 10.7% risk of major congenital malformations - nearly four times the background rate of 2.8%. Babies exposed to valproate are also at higher risk of autism and lower IQ scores. The good news? Lamotrigine and levetiracetam are far safer alternatives. Women with epilepsy who switch before conception reduce their baby’s risk of major defects from over 10% to under 3%.Safe Alternatives for Common Pregnancy Complaints
You don’t have to suffer. There are safe, effective ways to manage everyday issues:- Pain and fever: Acetaminophen - only when needed, at 325-650 mg every 4-6 hours, max 3,000 mg per day.
- Allergies: Loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra). All have strong safety data from over 2,000 exposed pregnancies.
- Congestion: Start with saline nasal spray. If you need more, pseudoephedrine (Sudafed) is okay after the first trimester - but avoid it if you have high blood pressure. Don’t use phenylephrine; it’s less effective and has less safety data.
- Constipation: Fiber (25-30 grams daily), water, and movement first. If you need meds, docusate sodium (Colace) or polyethylene glycol (Miralax) are both Category B and safe in over 700 documented cases.
- Heartburn: Calcium carbonate (Tums) or magnesium hydroxide (Milk of Magnesia) are safe. Avoid sodium bicarbonate (baking soda) - it can cause fluid overload.
What About Antidepressants?
This is one of the hardest decisions. Paroxetine (Paxil) increases the risk of heart defects from 0.7% to 1.5-2%. But untreated depression? That raises your risk of preterm birth by 64% and low birth weight by 73%. SSRIs like sertraline and citalopram are generally preferred over paroxetine. The risk of persistent pulmonary hypertension of the newborn (PPHN) goes from 1-2 per 1,000 to 5-6 per 1,000 with SSRIs - still low, but real. The bigger risk is relapse: 20-25% of women who stop their meds during pregnancy have a major depressive episode. That’s dangerous for both you and your baby. Work with your psychiatrist and OB. Don’t stop cold turkey. Adjusting slowly under supervision is safer than sudden withdrawal.
Warfarin and Other Blood Thinners
Warfarin (Coumadin) crosses the placenta and can cause fetal warfarin syndrome - facial deformities, bone problems, and intellectual disability. The risk is 6-10% if taken during the first trimester. The solution? Switch to low molecular weight heparin (like enoxaparin/Lovenox) before you get pregnant. Heparin doesn’t cross the placenta. It’s safe. You’ll need injections, but they’re far safer than warfarin. If you’re on warfarin for a mechanical heart valve, talk to a maternal-fetal medicine specialist - this requires expert management.What to Do Right Now
Don’t wait for your next prenatal visit. Take action today:- Make a full list of everything you take - prescriptions, OTC meds, vitamins, herbs, supplements.
- Check each one against the FDA’s Pregnancy and Lactation Labeling Rule (PLLR) details. You can find them on the FDA website or through MotherToBaby.
- Call your doctor or midwife. Don’t assume something is safe because it’s “over the counter.”
- If you’ve already taken a risky medication, don’t panic. Many exposures don’t lead to problems. But you need to get monitored.
Where to Get Trusted Help
MotherToBaby is a free, confidential service run by experts in pregnancy and medication safety. They’ve answered over 2.3 million questions annually. Their fact sheets are based on real data - not guesswork. Call them. Text them. Visit their website. They’re there to help you make informed choices, not scare you. The landscape of pregnancy medication safety is changing fast. What was safe last year might not be today. But you don’t have to navigate it alone. With the right information and support, you can protect your health - and your baby’s - without unnecessary fear.Is it safe to take Tylenol while pregnant?
Tylenol (acetaminophen) is still the preferred pain reliever during pregnancy, but only when used at the lowest effective dose for the shortest time possible. New research links prolonged use - especially throughout pregnancy - to higher risks of ADHD and autism in children. If you have a fever of 102°F or higher, treating it with acetaminophen is safer than leaving it untreated. Always check with your provider before using it regularly.
Can I take ibuprofen during pregnancy?
No, after 20 weeks of pregnancy. Ibuprofen and other NSAIDs can cause fetal kidney damage and dangerously low amniotic fluid, which can lead to serious complications. Even before 20 weeks, it’s best to avoid them unless your doctor specifically recommends low-dose aspirin for preeclampsia prevention. Use acetaminophen instead for pain or fever.
What’s the safest allergy medicine during pregnancy?
Loratadine (Claritin) and cetirizine (Zyrtec) are both Category B and have been studied in over 2,000 pregnancies with no increased risk of birth defects. Fexofenadine (Allegra) is also considered safe. Avoid first-generation antihistamines like diphenhydramine (Benadryl) if possible - they can cause drowsiness and may cross into the baby’s system more easily.
Is it safe to take antibiotics while pregnant?
Some are, some aren’t. Penicillins like amoxicillin and cephalosporins like cephalexin are safe. Avoid tetracyclines (doxycycline) and fluoroquinolones (ciprofloxacin) - they can damage developing bones and teeth. Always confirm with your provider before taking any antibiotic, even if it’s for a common infection like a UTI.
What should I do if I took a risky medication before knowing I was pregnant?
Don’t panic. Many exposures don’t result in birth defects. Call MotherToBaby or your OB/GYN right away. They’ll assess the timing, dosage, and medication to determine your actual risk. You may need extra ultrasounds or monitoring, but most pregnancies continue without issues. The key is early awareness - not guilt.
Are herbal supplements safe during pregnancy?
Many are not. Herbal products are not regulated like medications, and safety data is often lacking. Some herbs like black cohosh, goldenseal, and pennyroyal can trigger contractions or affect fetal development. Always tell your provider about every supplement you take - even if you think it’s “natural.”

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.