When opioids and benzodiazepines are taken together, the risk of stopping breathing doesn’t just go up-it multiplies. This isn’t a theoretical concern. It’s happening every day in homes, clinics, and emergency rooms across the country. The FDA issued its first official warning about this combination in 2016, and by 2019, they strengthened it with a Boxed Warning-the most serious type of alert a drug label can carry. The message was clear: mixing these drugs can lead to extreme sleepiness, slowed or stopped breathing, coma, or death.
Why This Combination Is So Dangerous
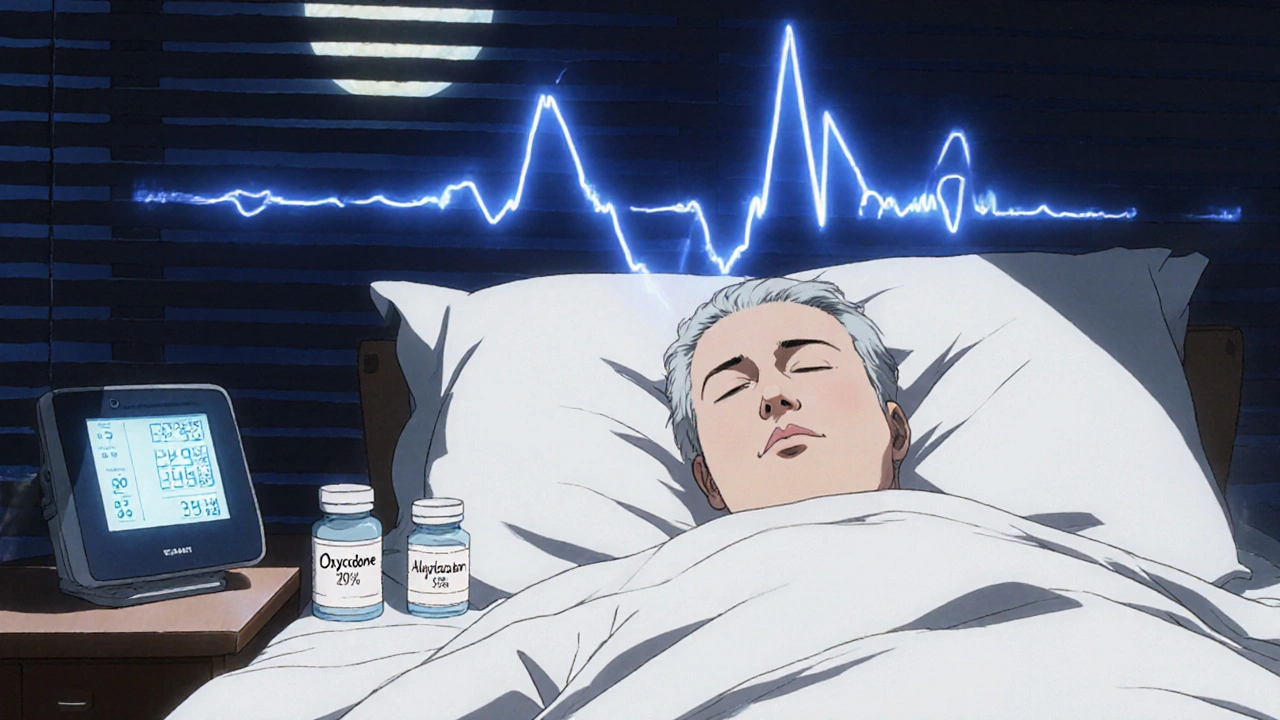
Opioids like oxycodone, hydrocodone, and fentanyl work by binding to mu-opioid receptors in the brainstem, the part of your brain that controls automatic breathing. Benzodiazepines like alprazolam, lorazepam, and diazepam boost the effect of GABA, a calming neurotransmitter that also slows down brain activity, including the signals that tell you to breathe. Alone, each drug can suppress breathing. Together, they don’t just add up-they multiply. Studies show that when taken in combination, the risk of respiratory depression is far greater than the sum of each drug’s individual effect.A 2021 review in the Annals of Palliative Medicine found that patients on both drugs experienced oxygen levels dropping below 90% in 85% of cases-compared to just 45% when taking opioids alone. This isn’t just about feeling sleepy. It’s about your body losing the ability to respond to rising carbon dioxide levels, which normally trigger you to take a deeper breath. In sleep, when your body is already relaxed, this failure can be fatal.
Who’s Most at Risk
It’s not just people who misuse drugs. Many patients are prescribed both medications by different doctors for separate conditions: one for chronic pain, another for anxiety or insomnia. Older adults are especially vulnerable. The American Geriatrics Society includes this combination in its Beers Criteria-a list of potentially inappropriate medications for seniors-because of the high risk of falls and respiratory failure. Even people who’ve been on opioids for years aren’t safe. Chronic opioid use builds tolerance to pain relief and euphoria, but not to respiratory depression from benzodiazepines. That means someone who’s been on opioids for years might think they’re “used to” sedation, but a new benzodiazepine prescription can still shut down their breathing.People on methadone or extended-release opioids are at even higher risk. These drugs stay in the body longer, and when combined with benzodiazepines that block the CYP3A4 liver enzyme (like alprazolam), opioid levels can spike unexpectedly. One study showed that patients on both drugs had a 10 times higher chance of dying from overdose than those taking opioids alone.
The Numbers Don’t Lie
The CDC reports that in 2020, 16% of all opioid-related overdose deaths involved benzodiazepines. That’s roughly 220 Americans dying each day from opioid overdoses-and nearly 1 in 6 of those deaths included a benzodiazepine. Between 1999 and 2017, the rate of overdose deaths involving both drug classes jumped from 0.6 to 8.8 per 100,000 people. Even though that number has dipped slightly since, it’s still far higher than it was two decades ago.A 2021 study in JAMA Network Open found that 15% of Medicare Part D patients on long-term opioids were also prescribed benzodiazepines. Alarmingly, 4.3% of those were on high-risk combinations: long-acting benzodiazepines with extended-release opioids. These are the exact pairs that linger in the body longest, increasing the chance of a fatal buildup.

What Doctors Are Told to Do
The FDA’s guidance is strict: avoid prescribing these drugs together unless absolutely necessary. If there’s no alternative, start with the lowest possible dose of the benzodiazepine and monitor the patient closely for signs of sedation or breathing trouble. For patients already taking both, the recommendation isn’t to quit cold turkey-it’s to taper slowly under supervision. Abruptly stopping either drug can trigger seizures (in the case of benzodiazepines) or severe withdrawal symptoms like vomiting, sweating, and rapid heart rate (with opioids).Doctors are also urged to warn patients and their caregivers. Many people don’t realize that even a single extra dose of a benzodiazepine-say, taking an extra Xanax because they couldn’t sleep-can turn a safe regimen deadly when opioids are already in their system. The FDA specifically advises clinicians to tell patients: “If you feel unusually drowsy, have trouble breathing, or feel confused after taking these together, seek help immediately.”
What You Should Do If You’re Taking Both
If you’re on opioids and benzodiazepines, don’t panic-but do act. First, talk to your doctor. Ask if there’s a safer alternative for your anxiety, insomnia, or muscle spasms. Non-addictive options like cognitive behavioral therapy, melatonin, or certain antidepressants may work just as well without the breathing risk.Never increase your dose on your own. Don’t mix these drugs with alcohol, sleep aids, or even over-the-counter cold medicines that cause drowsiness. Keep naloxone (Narcan) on hand if you’re at risk for overdose-it won’t reverse benzodiazepine effects, but it can help if opioids are the main cause of respiratory failure.
Make sure someone in your household knows the signs of overdose: slow or shallow breathing, unresponsiveness, blue lips or fingernails, and extreme drowsiness. If you see these, call emergency services immediately and administer naloxone if available.
What’s Being Done to Stop This
Health systems are starting to catch up. Electronic health records now often include automated alerts when a prescriber tries to write a prescription for both drugs. One study showed these alerts reduced dangerous co-prescribing by 27.3% in a major U.S. health network. The CDC funded research in 2022 to better understand why this combination is so deadly and how to predict who’s most at risk. Some hospitals now require mandatory counseling before prescribing benzodiazepines to patients on opioids.Research is also exploring new pain medications that don’t affect breathing. Non-opioid alternatives like gabapentin, certain NSAIDs, and nerve blocks are gaining ground. For anxiety, non-benzodiazepine options like buspirone or SSRIs are being promoted more aggressively.
Final Reality Check
This isn’t about fearmongering. It’s about facts. The science is clear: combining opioids and benzodiazepines dramatically increases the chance of dying from respiratory failure. It’s not rare. It’s not isolated. It’s a pattern that’s been documented for years, yet it continues because of fragmented care, lack of communication between providers, and patient misunderstanding.If you or someone you know is taking both, don’t wait for a crisis to act. Talk to your doctor. Ask for a medication review. Explore alternatives. Keep naloxone nearby. And never assume that because you’ve taken these drugs before, you’re safe. The body doesn’t build tolerance to the silent, deadly effect they have on your breath.
Can I take opioids and benzodiazepines if my doctor prescribes them?
Only if no other option exists and your doctor has thoroughly explained the risks. Even then, you should start with the lowest possible doses and be monitored closely. The FDA recommends avoiding this combination whenever possible. If you’re already taking both, do not stop suddenly-work with your provider on a safe taper plan.
How do I know if I’m experiencing respiratory depression?
Signs include breathing that’s slower than 10 breaths per minute, shallow breathing where your chest barely moves, extreme drowsiness you can’t wake up from, confusion, bluish lips or fingertips, and inability to stay awake. If you notice any of these, especially after taking both drugs, call emergency services right away.
Does naloxone reverse the effects of benzodiazepines?
No, naloxone only reverses opioid effects. It won’t fix breathing problems caused by benzodiazepines. But if opioids are part of the mix-like in most overdose cases-naloxone can still save your life by restoring breathing. Always keep it on hand if you’re using opioids, even if you’re also taking benzodiazepines.
Are there safer alternatives to benzodiazepines for anxiety or insomnia?
Yes. For anxiety, SSRIs like sertraline or escitalopram are often effective and don’t cause respiratory depression. For insomnia, non-addictive options include cognitive behavioral therapy for insomnia (CBT-I), melatonin, or medications like trazodone or ramelteon. Talk to your doctor about switching-many people find these alternatives work well without the overdose risk.
Why do doctors still prescribe both if it’s so dangerous?
Sometimes, it’s because patients have multiple providers-one for pain, another for mental health-and communication breaks down. Other times, doctors feel pressured to treat symptoms quickly, and benzodiazepines seem like an easy fix. But awareness is growing. Many clinics now require joint reviews before prescribing both, and electronic alerts are helping reduce dangerous combinations.
Can I stop taking one of these drugs on my own?
No. Stopping benzodiazepines suddenly can cause seizures, and stopping opioids abruptly can trigger severe withdrawal symptoms like vomiting, diarrhea, rapid heart rate, and intense anxiety. Always work with your doctor to create a slow, supervised taper plan. Abrupt changes can be life-threatening.
Is this risk higher for older adults?
Yes. Older adults are more sensitive to the sedative effects of both drugs. Their metabolism slows down, so drugs stay in their system longer. They’re also more likely to have other health conditions that affect breathing, like COPD or sleep apnea. The American Geriatrics Society specifically lists this combination as potentially inappropriate for seniors due to the high risk of falls and respiratory failure.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.