When a doctor prescribes a generic drug, most patients assume it’s just as safe and effective as the brand-name version. After all, the FDA says so. But behind the scenes, many clinicians are starting to ask harder questions - especially when the pill comes from a factory halfway across the world.
Why are doctors worried?
Generic drugs make up over 90% of prescriptions in the U.S. They’re cheaper, widely available, and legally required to match brand-name drugs in active ingredients. But here’s the catch: they don’t have to be made in the same place, by the same company, or under the same conditions. A 2023 study from Ohio State University looked at over 1.5 million adverse event reports in the FDA’s database. What they found shocked even seasoned pharmacists. Generic drugs manufactured in India were linked to a 54% higher rate of severe side effects - including hospitalizations, permanent disability, and death - compared to identical generics made in the U.S. The difference wasn’t random. It showed up most clearly in older, low-cost generics that had been on the market for years, where price pressure had squeezed margins thin. "As drugs get cheaper and cheaper and the competition gets more intense to hold down costs," said lead researcher Professor Robert S. Gray, "you start to see corners cut in operations and supply chains. That’s when quality slips."How a pill becomes a problem
A single generic pill might pass through six different factories before it reaches your medicine cabinet. The active ingredient? Made in a chemical plant in Gujarat. The filler? Mixed in a facility in Pennsylvania. The coating? Applied in Mexico. The blister pack? Printed in China. Only one name appears on the label - and it’s often not the company that actually made the most critical parts. The FDA requires generics to prove they’re bioequivalent: meaning they release the same amount of active drug into the bloodstream at the same rate as the brand-name version. That sounds solid - until you learn how inspections work. In the U.S., FDA inspectors show up unannounced. They walk through labs, check equipment logs, and test samples on the spot. In India and China? Inspections are scheduled weeks in advance. Manufacturers know exactly when they’re coming. They clean up. They fix what’s broken. They hide what isn’t. "It’s like giving a restaurant a heads-up before a health inspection," said one pharmacist who’s worked in supply chain compliance for 18 years. "You don’t find the real problems. You find the ones they want you to see."What’s really at stake?
It’s not just about side effects. It’s about access. Drug shortages - the kind that force oncologists to delay cancer treatments or hospitals to ration insulin - are increasingly tied to manufacturing failures. Duke-Margolis Center research shows that over 60% of drug shortages since 2018 were caused by quality issues at overseas facilities. Many of those drugs are old, cheap generics that no one wants to invest in… until something breaks. A single failed batch of a generic blood thinner can ripple through hospitals for months. Patients get switched to alternatives - sometimes less effective, sometimes more expensive. Nurses scramble. Doctors worry. And patients? They just get sicker. One nurse in Ohio described a case where a patient on a generic version of warfarin started having unexplained bleeding. Her INR levels - which measure blood clotting - kept spiking. The brand-name version had worked fine for years. The generic? Same active ingredient. Same dosage. But when they switched back to the brand, the bleeding stopped. No other changes. Just the pill.
Is the FDA doing enough?
The FDA says the U.S. drug supply is among the safest in the world. They point to over 1,300 staff in their Office of Pharmaceutical Quality and their inspections of more than 3,000 foreign facilities each year. But here’s the problem: they can’t be everywhere at once. And they can’t force foreign manufacturers to change their practices. Even when violations are found - like unclean equipment, falsified data, or substandard raw materials - penalties are rare. Fines are small. And the manufacturer? They just move production to another facility and keep going. The FDA doesn’t label where a drug was made on the bottle. Patients and doctors have no way to know if the generic they’re taking came from a facility with a history of violations - or one that just passed a scheduled inspection after cleaning up for a week.Could American-made generics be the answer?
There’s a growing push to bring generic manufacturing back to the U.S. The University of Wisconsin School of Pharmacy argues that domestic production could reduce shortages, improve quality control, and stabilize the supply chain. Advanced manufacturing technologies - like continuous production and real-time quality monitoring - are already being used by U.S. companies. These systems catch problems as they happen, not months later after patients get sick. Over 80% of drugs made with these technologies are produced in the U.S. The catch? They cost more to set up. A single advanced manufacturing line can run $50 million. For companies making pennies per pill, that’s a hard sell. So they keep outsourcing. But what if we changed the rules? Some experts, including the Ohio State researchers, suggest the FDA should start publishing manufacturing locations on drug labels - not as a scare tactic, but as a transparency tool. Imagine if your prescription said: "Made in India" or "Made in Ohio." Would you choose differently? Would insurers pay more for higher-quality versions? "We need a market where quality is rewarded, not punished," said Dr. Iyer, a pharmacist and drug policy researcher. "Right now, the cheapest bid wins. That’s not how you build a safe medicine supply."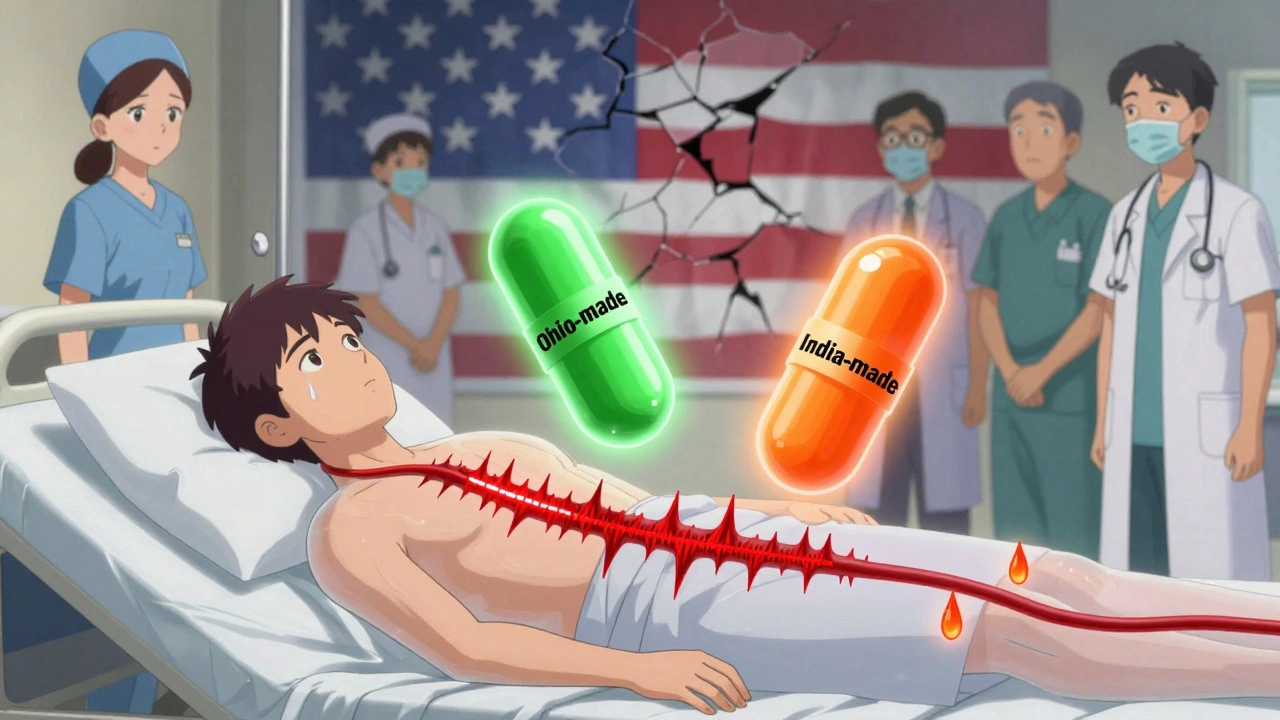
What can clinicians do?
Doctors and pharmacists aren’t powerless. Here’s what’s working right now:- When a patient has unexplained side effects or lab abnormalities, ask: "Has the generic brand changed?" Many times, it has - and it’s the hidden culprit.
- Keep a list of generics that have caused issues in your practice. Share it with your pharmacy. Ask them to stick with reliable suppliers.
- When possible, request brand-name drugs for critical medications - like thyroid meds, seizure drugs, or blood thinners - where small differences in absorption can be dangerous.
- Support policies that incentivize domestic manufacturing. It’s not just about patriotism. It’s about reliability.
The bigger picture
This isn’t just about pills. It’s about trust. Patients trust that their medicine will work. Clinicians trust that the system is watching out for them. But when quality slips through the cracks - when a patient dies after switching to a cheaper generic - that trust breaks. The FDA isn’t broken. But it’s stretched too thin. The global supply chain works - until it doesn’t. And when it fails, it’s not a factory in India or China that pays the price. It’s the patient on the other end of the prescription. The solution won’t come from one law or one inspection. It will come from transparency, accountability, and a willingness to pay a little more for safety. Because in medicine, the cheapest option isn’t always the best. Sometimes, it’s the most dangerous.Are generic drugs always safe?
Most generics are safe and effective. But not all are made equally. A 2023 study found that generics manufactured in India had a 54% higher rate of severe adverse events compared to those made in the U.S. The difference comes down to manufacturing standards, inspection practices, and cost pressures - not the active ingredient.
Why do some generics cause more side effects?
The active ingredient is the same, but the fillers, coatings, and how the drug is released can vary. These differences affect how quickly the body absorbs the medicine. In older, low-cost generics, manufacturers may use cheaper materials or skip quality checks to keep prices down. This can lead to inconsistent dosing - too much or too little - which triggers side effects or reduces effectiveness.
Can I tell where my generic drug was made?
Not from the label. The FDA doesn’t require manufacturers to list the country of origin on prescription bottles. Even the pharmacy often doesn’t know. Some specialty pharmacies track this information internally, but most don’t. If you’re concerned, ask your pharmacist - but be prepared for them to say they don’t have the data.
Should I avoid all generic drugs?
No. Many generics are safe and save patients thousands of dollars. But for critical medications - like blood thinners, epilepsy drugs, thyroid hormones, or immunosuppressants - even small variations can be risky. If you’ve had issues with a generic, ask your doctor about switching brands or requesting the brand-name version. Your health isn’t a commodity.
Is the FDA planning to fix this?
The FDA has proposed making manufacturing location more transparent and is investing in advanced manufacturing technologies. But they still conduct scheduled inspections overseas, which experts say allows manufacturers to hide problems. Real change would require unannounced global inspections and financial incentives for U.S.-based production - neither of which is guaranteed.
Why don’t pharmacies just use U.S.-made generics?
Because they’re often more expensive. Pharmacy benefit managers and insurers choose the lowest-cost option to save money. A generic made in the U.S. might cost 30-50% more than one made in India. In a system driven by price, quality often loses. Some hospitals and clinics are starting to prioritize quality over cost - but they’re still the exception.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.