Stress Impact on Fertility Calculator
Low Stress
Cortisol: 5-20 µg/dL
GnRH: Normal
Ovulation: Regular
Moderate Stress
Cortisol: 21-30 µg/dL
GnRH: Occasional Dip
Ovulation: Slight Irregularity
High Stress
Cortisol: >30 µg/dL
GnRH: Suppressed
Ovulation: Anovulatory Risk
Your Results
With a stress level of 15, your cortisol is likely in the moderate range (21-30 µg/dL). This may cause occasional GnRH dips, potentially leading to slight ovulation irregularity.
Recommended Actions
- Practice 10-minute mindfulness meditation daily
- Limit caffeine after noon
- Maintain regular sleep schedule (7-8 hours)
- Engage in moderate aerobic exercise (30 minutes, 4-5 times/week)
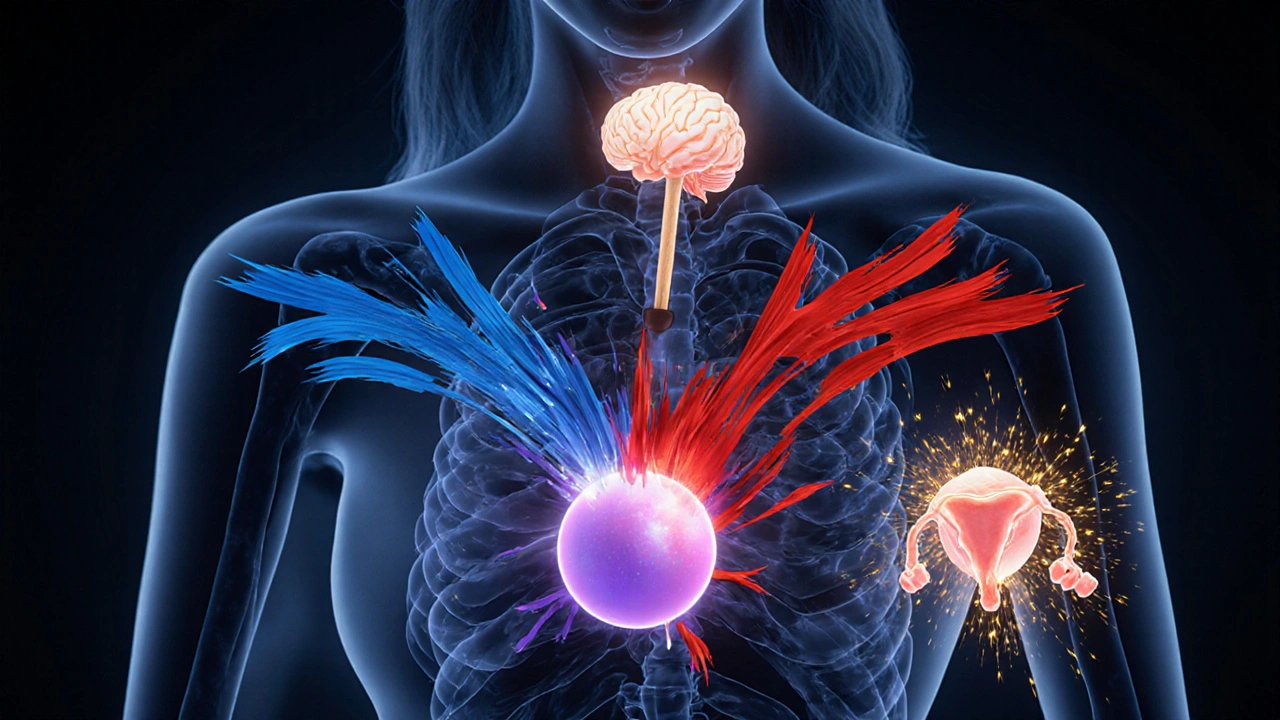
When it comes to getting pregnant, stress is a physiological and psychological response to perceived challenges that triggers a cascade of hormones in the body. Most people think of stress as just feeling frazzled, but the hormonal ripple effect can actually shift the timing of ovulation and lower the odds of conception. Let’s walk through what really happens, why it matters, and what you can do to keep stress from stealing your baby‑making window.
What Stress Does to Your Hormone Orchestra
The body’s stress response is driven primarily by the cortisol hormone. When stress spikes, cortisol shoots up, and that surge talks to the brain’s hypothalamus, which controls the release of gonadotropin‑releasing hormone (GnRH). GnRH is the maestro that cues the pituitary to produce luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). Both LH and FSH are essential for follicle development and the release of a mature egg.
In a low‑stress scenario, cortisol stays in a healthy range (5‑20 µg/dL in the morning) and lets GnRH fire on a regular schedule. But under chronic or high stress, cortisol can stay elevated for hours, even days. That persistent elevation can:
- Suppress GnRH pulses, leading to lower LH and FSH bursts.
- Shift the timing of the luteal phase, making the fertile window harder to predict.
- Increase the production of prolactin, which can directly inhibit ovulation.
How Ovulation Gets Disrupted
Ovulation is the release of a mature egg from the ovarian follicle, typically around day 14 of a 28‑day menstrual cycle. The timing is tightly linked to the ebb and flow of LH and FSH. When stress interferes with those hormones, you might see:
- Irregular cycle lengths - cycles can shorten to 21 days or lengthen beyond 35 days.
- Anovulatory cycles - no egg released at all, which can happen up to 20% of cycles in highly stressed women.
- Shifted LH surge - the spike that triggers ovulation may occur earlier or later, confusing natural tracking methods.
Impact on Conception Odds
The moment an egg is released, the clock starts ticking. Sperm can survive up to five days, but the egg is viable for only about 24 hours. If stress pushes ovulation out of the predicted window, you might miss the optimal timing for intercourse, dropping the chance of fertilization. A 2023 longitudinal study of 1,200 couples trying to conceive found that women reporting high chronic stress (Perceived Stress Scale score > 25) had a 30% lower probability of pregnancy within the first six months compared with low‑stress peers. The same study noted that stress‑related hormonal changes also reduced uterine lining thickness, making implantation less likely.
Other Health Factors That Can Compound Stress Effects
Stress rarely acts alone. It often teams up with other conditions that already threaten fertility:
- Polycystic Ovary Syndrome (PCOS) is a hormonal disorder characterized by excess androgen and irregular ovulation - stress can worsen insulin resistance, amplifying PCOS symptoms.
- Thyroid disorders affect metabolism and can disrupt menstrual regularity - cortisol overload can further unbalance thyroid hormones.
- Weight fluctuations - stress‑induced cortisol promotes abdominal fat, which can impair ovulation.
Practical Ways to Keep Stress from Sabotaging Fertility
Below is a quick‑start toolkit you can adopt today. The goal is to lower cortisol, stabilize GnRH pulses, and give your body a clear, predictable fertile window.
| Stress Level | Typical Hormonal Change | Recommended Action |
|---|---|---|
| Low (Score 0‑10) | Normal cortisol (5‑20 µg/dL), regular GnRH | Maintain routine; regular exercise, balanced diet. |
| Moderate (Score 11‑20) | Slightly elevated cortisol (21‑30 µg/dL), occasional GnRH dip | Introduce 10‑min mindfulness meditation daily; limit caffeine after noon. |
| High (Score 21+) | Chronically high cortisol (>30 µg/dL), suppressed GnRH, lower LH/FSH | Seek therapist or counselor; practice yoga or tai chi 3×/week; ensure 7‑8h sleep. |
Other evidence‑backed strategies include:
- Sleep hygiene: Aim for 7‑8 hours; deep sleep reduces nighttime cortisol spikes.
- Physical activity: Moderate aerobic exercise (30min, 4‑5times/week) balances stress hormones without overtraining, which can raise cortisol.
- Nutrition: Foods rich in omega‑3 fatty acids (salmon, walnuts) and magnesium (leafy greens, pumpkin seeds) support adrenal health.
- Mind‑body practices: Guided imagery, progressive muscle relaxation, or even simple deep‑breathing (4‑7‑8 technique) can shave 5‑10µg/dL off cortisol within weeks.
Tracking both stress and ovulation can help you see patterns. Use a journal or a fertility‑tracking app that lets you log mood, sleep, and any stressful events alongside basal body temperature or LH‑strip results.

When to Seek Professional Help
If you’ve been trying to conceive for six months (or three months if you’re over 35) and notice persistent cycle irregularities, it’s time to talk to a reproductive endocrinologist. They may run tests such as:
- Serum cortisol (morning and afternoon)
- LH and FSH panels on day3 of the cycle
- Thyroid‑stimulating hormone (TSH) and free T4
- Anti‑Müllerian hormone (AMH) to gauge ovarian reserve
Bottom Line: Stress Isn’t Destiny
While chronic stress can throw off the delicate hormonal choreography that drives ovulation and implantation, it’s also one of the most modifiable factors you control. By recognizing the signs, monitoring hormone trends, and adopting proven stress‑reduction habits, you give your body the best chance to release a healthy egg and welcome a pregnancy.
Frequently Asked Questions
Can occasional stress really affect ovulation?
A one‑off stressful event may cause a temporary cortisol spike, but it usually doesn’t disrupt the entire cycle. Chronic or repeated stress, however, can blunt GnRH pulses enough to delay or skip ovulation.
How long does it take for stress‑reduction techniques to improve fertility?
Most women see measurable drops in cortisol within 2‑4weeks of consistent practice (e.g., daily meditation). Ovulation patterns often normalize after one to two full cycles once stress levels are under control.
Is it safe to take supplements to lower cortisol while trying to conceive?
Supplements like phosphatidylserine or ashwagandha have shown modest cortisol‑lowering effects, but you should discuss any new supplement with your fertility specialist, especially during pre‑conception.
Can stress affect the uterine lining as well as ovulation?
Yes. Elevated cortisol can reduce blood flow to the endometrium and lower estrogen levels, leading to a thinner lining that’s less receptive to implantation.
Should my partner’s stress be considered in our fertility plan?
Male stress can lower testosterone and sperm quality, so it’s wise for both partners to manage stress together. Joint activities like walks or yoga can improve outcomes for both.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.