For decades, taking a daily low-dose aspirin was one of the most common things people did to protect their hearts. If your parent or grandparent had a heart attack, chances are they were told to pop a baby aspirin every morning. But today, that advice has changed-dramatically. As of 2026, aspirin therapy is no longer a one-size-fits-all solution for preventing heart disease. In fact, for most healthy adults, it may do more harm than good.
Why the Rules Changed
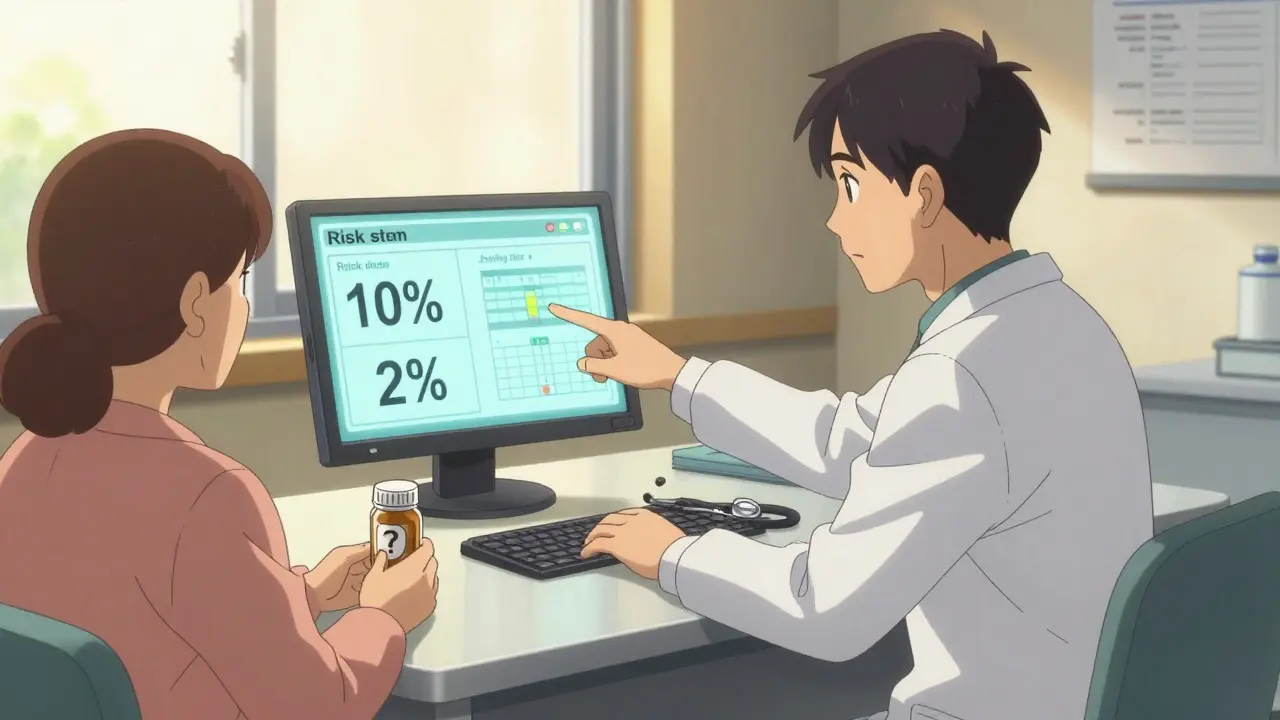
The shift didn’t happen overnight. Over the last 15 years, massive studies involving more than 130,000 people showed something surprising: while aspirin does reduce the chance of a first heart attack or stroke by a small amount, it also increases the risk of serious, sometimes life-threatening bleeding. This includes bleeding in the stomach, intestines, and brain. For people with no history of heart disease, the math just doesn’t add up anymore.Back in the 1990s and early 2000s, aspirin was seen as a miracle drug for prevention. But today, we have better tools. Statins lower cholesterol more effectively. Blood pressure meds control hypertension. Diabetes is managed earlier. Lifestyle changes-like quitting smoking, eating better, and moving more-have become standard. These interventions cut heart disease risk by 25% to 37%. Aspirin? It cuts it by about 10% to 15%. And the bleeding risk stays the same.
The U.S. Preventive Services Task Force (USPSTF) updated its guidelines in 2022, and now says: Don’t start aspirin for heart disease prevention if you’re 60 or older. For people between 40 and 59, it’s not a blanket recommendation. You need to sit down with your doctor and weigh your personal risks.
Who Might Still Benefit
There are exceptions. Aspirin isn’t off the table for everyone. It’s still strongly recommended for people who’ve already had a heart attack, stroke, stent, or bypass surgery. That’s called secondary prevention, and it saves lives.For primary prevention-meaning you’ve never had a heart problem-there are two groups where aspirin might still make sense:
- Adults aged 40-59 with a 10% or higher 10-year risk of heart disease. This isn’t just about age. Your risk is calculated using your age, sex, race, blood pressure, cholesterol levels, whether you have diabetes, and if you smoke. If your score hits 10% or more, and you have no major bleeding risks, aspirin might be worth considering.
- People with type 2 diabetes and other risk factors. The American Diabetes Association still says aspirin can be considered for adults over 40 with diabetes who also have high blood pressure, high cholesterol, or smoke. Their risk of heart disease is so high that the potential benefit may still outweigh the risk.
One special case: people with familial hypercholesterolemia-a genetic condition that causes extremely high cholesterol from birth. Even if they’re young, their heart attack risk is so elevated that many lipid specialists still recommend aspirin, alongside statins.
The Bleeding Risk You Can’t Ignore
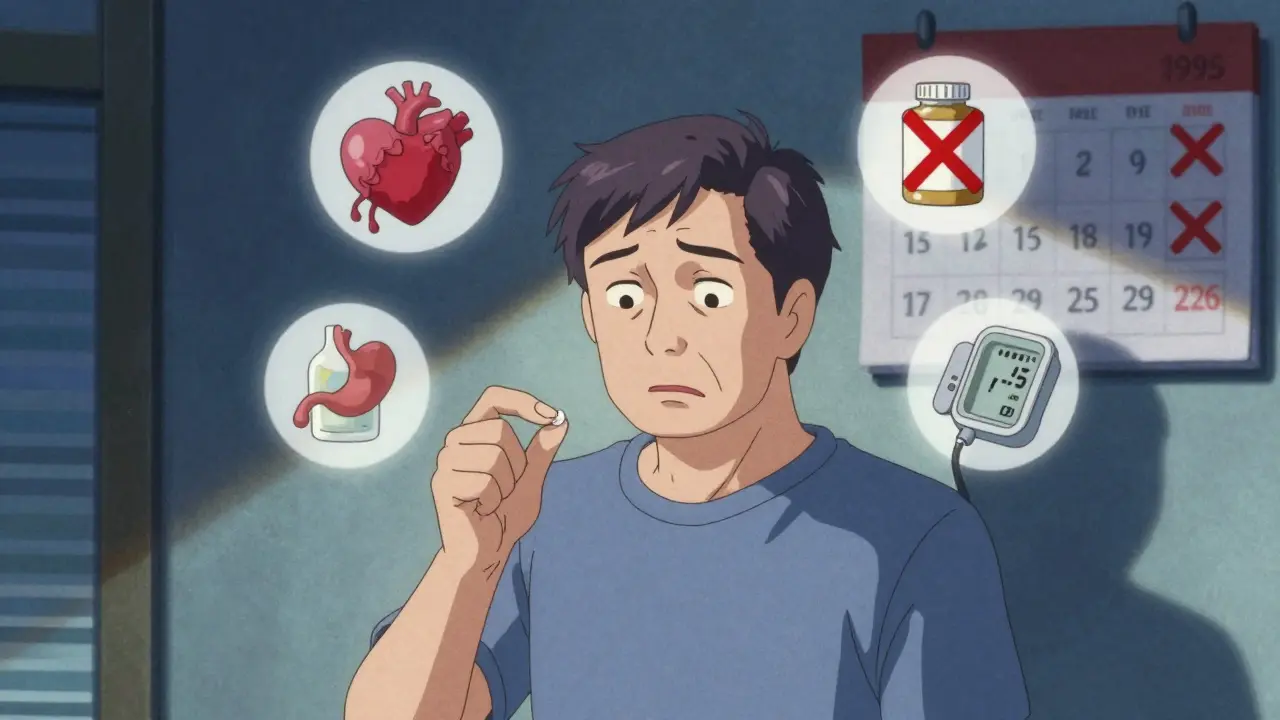
Aspirin works by thinning your blood. That’s why it helps prevent clots. But that same effect can cause bleeding-sometimes silently, sometimes suddenly.Studies show that for every 100 people like you who take aspirin daily for 10 years:
- 1 person might avoid a nonfatal heart attack
- 1 person might avoid a nonfatal stroke
- 2 people will have a major bleeding event
Major bleeding means you need hospitalization, a blood transfusion, or surgery. It’s not just a nosebleed or a bruise. It’s internal bleeding that can be fatal.
Who’s at highest risk? People with:
- A history of stomach ulcers or GI bleeding
- High blood pressure that’s not well controlled
- Kidney or liver disease
- Use of blood thinners like warfarin, apixaban, or rivaroxaban
- Regular alcohol use (more than 3 drinks a day)
- Age 60 or older
Doctors use a tool called the HAS-BLED score to assess bleeding risk. A score of 3 or higher means your bleeding risk is too high for aspirin. If you’ve ever had a bleed, you’re probably not a candidate.
What Dose Should You Take?
If your doctor says aspirin is right for you, the dose matters. There’s no benefit to taking more than 75-100 mg per day. That’s one low-dose, or “baby,” aspirin. Higher doses don’t work better-they just increase bleeding risk.Don’t assume over-the-counter aspirin is safe just because it’s cheap. A 3-month supply of generic 81 mg aspirin costs about $4-$6 in the U.S. But cost isn’t the issue. It’s the risk. Taking aspirin daily for years without medical supervision is like driving without a seatbelt-you might be fine, but the odds aren’t in your favor.
What About Family History?
This is the most common reason people keep taking aspirin even when they shouldn’t. “My dad had a heart attack at 58,” they say. “I don’t want that to happen to me.”Family history matters-but not the way most people think. If your father had a heart attack at 58, your risk is higher than average. But that doesn’t automatically mean you need aspirin. Your actual risk depends on your own numbers: your cholesterol, blood pressure, weight, and lifestyle. A 65-year-old with perfect blood pressure, normal cholesterol, and no diabetes has a much lower risk than a 55-year-old with high blood pressure, smoking, and high LDL.
One study found that nearly 70% of people over 60 who take aspirin for prevention do so because of family history-not because their doctor recommended it. That’s a dangerous assumption. Genetics load the gun. Lifestyle pulls the trigger. Aspirin doesn’t erase your genes.
What Should You Do Now?
If you’re currently taking aspirin daily and have never had heart disease, here’s what to do:- Don’t stop cold turkey. Stopping aspirin suddenly can trigger a rebound effect that slightly increases clot risk for a few days. Talk to your doctor first.
- Ask for your 10-year heart disease risk score. Request the ACC/AHA Pooled Cohort Equation. It’s easy to calculate. Your doctor should have it in your electronic record.
- Ask about bleeding risk. Do you have a history of ulcers? Are you on other blood thinners? Do you drink alcohol regularly?
- Ask what alternatives exist. Are you on a statin? Is your blood pressure under control? Have you quit smoking? These are far more powerful than aspirin.
If you’re under 40, aspirin is almost never recommended for prevention. If you’re over 70, it’s actively discouraged. The only group where the balance might still tip toward benefit is middle-aged adults with high risk and low bleeding risk-and even then, it’s not automatic.

What’s Replacing Aspirin?
The real winner in heart disease prevention isn’t a drug-it’s a strategy. Statins are now the first-line treatment for most people with elevated cholesterol or diabetes. They cut heart attack risk by up to 37%. Blood pressure control cuts it by 20-30%. Exercise, Mediterranean-style eating, and weight loss are just as powerful.Aspirin’s role is shrinking. In 2010, 40% of adults aged 40-75 took it for prevention. By 2022, that dropped to 22%. The Veterans Health Administration cut inappropriate aspirin use by 37% in just three years by changing protocols and educating doctors.
Even the FDA has weighed in. In 2014, they denied a request to approve aspirin for preventing first heart attacks because the evidence didn’t show enough benefit to justify the risk.
Final Thoughts
Aspirin isn’t evil. It’s a powerful tool. But like any tool, it’s only useful in the right hands. For people with established heart disease, it’s life-saving. For healthy people trying to prevent their first event, it’s often unnecessary-and risky.The goal isn’t to take more pills. It’s to live healthier. Control your blood pressure. Lower your cholesterol. Move every day. Eat real food. Don’t smoke. Those things do more than any pill ever could.
If you’re unsure whether you should keep taking aspirin, don’t guess. Talk to your doctor. Bring your numbers. Ask for the facts. Your heart isn’t worth risking for an outdated habit.
Should I take aspirin every day to prevent a heart attack if I’m healthy?
For most healthy adults, no. The risk of serious bleeding-especially after age 60-usually outweighs the small benefit of preventing a first heart attack. Aspirin is no longer recommended for routine prevention in people without heart disease. Always talk to your doctor before starting or stopping.
Is baby aspirin safer than regular aspirin?
Yes, but only in terms of dose. Low-dose aspirin (75-100 mg, often called baby aspirin) is the only form recommended for prevention. Regular aspirin (325 mg) offers no extra benefit and increases bleeding risk. Never take more than 100 mg daily for prevention unless your doctor specifically tells you to.
Can I take aspirin if I have diabetes?
Maybe. For adults with type 2 diabetes over 40 who also have other risk factors like high blood pressure or smoking, aspirin may still be considered. But if you’re over 70 or have a history of bleeding, it’s usually not recommended. Your doctor will calculate your overall risk before deciding.
What if I’ve been taking aspirin for years-should I stop?
Don’t stop on your own. If you’re over 60 and have no history of heart disease, you’re likely better off stopping. But stopping suddenly can carry a small risk of rebound clotting. Talk to your doctor. They can help you taper safely if needed and assess whether you still need it.
Does aspirin help prevent strokes too?
It can reduce the risk of ischemic strokes (caused by clots) by about 12%, but it doesn’t help with hemorrhagic strokes (caused by bleeding). In fact, it increases the risk of those. For people with no prior stroke, the overall benefit is minimal and often outweighed by bleeding risks.
Are there natural alternatives to aspirin for heart health?
There’s no natural substitute that works like aspirin to block platelets. But lifestyle changes are far more effective: eating omega-3-rich foods, exercising regularly, controlling blood pressure, and managing cholesterol with diet and statins all reduce heart disease risk more than aspirin ever could. Supplements like fish oil or garlic don’t replace medical therapy.
Next Steps
If you’re taking aspirin for prevention:- Ask your doctor for your 10-year heart disease risk score.
- Review your bleeding risk factors: ulcers, alcohol, other medications.
- Confirm whether you’re on a statin-and if your cholesterol is under control.
- If you’re over 60 and have no heart disease, discuss stopping aspirin.
If you’re not taking aspirin but are worried about heart disease:
- Get your blood pressure, cholesterol, and blood sugar checked.
- Ask about a coronary calcium scan if you’re over 45 and have family history.
- Focus on lifestyle. It’s the most powerful prevention tool you have.
Aspirin isn’t the hero it once was. But good health still is.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.