When your shoulder aches after lifting, your knee hurts when you kneel, or your heel burns after a long walk, it’s easy to blame it all on "arthritis" or "overuse." But if you’ve been told you have bursitis or tendinitis, you’re dealing with two very different problems - even though they feel similar. Both cause pain near joints, both get worse with movement, and both are common after 40. But treating them the same way can make things worse. Knowing the difference isn’t just academic - it changes how you recover.
What’s the Real Difference Between Bursitis and Tendinitis?
Bursitis is inflammation of a bursa. These are small, fluid-filled sacs that act like cushions between bones and tendons or muscles. There are about 160 of them in your body, and the most common trouble spots are the shoulder, elbow, hip, and knee. When a bursa gets irritated - from repeated pressure, a fall, or even just old age - it swells up and becomes painful. The pain tends to be more spread out, like a dull ache around the joint, and it often flares up when you lie on the sore side at night.
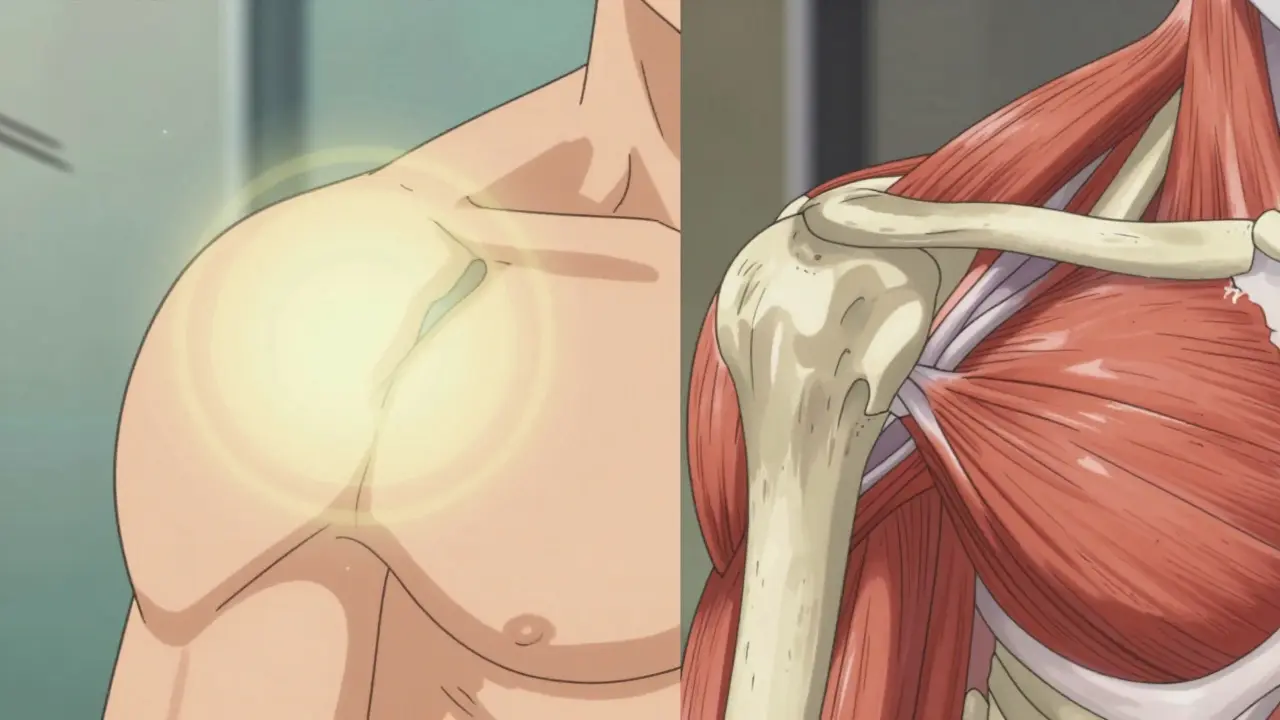
Tendinitis, on the other hand, is inflammation of a tendon. Tendons are the tough cords that connect your muscles to your bones. When you move, your muscles pull on these cords. If you do the same motion too often - typing, swinging a racket, lifting boxes - the tendon gets irritated. The pain from tendinitis doesn’t just sit there. It follows the path of the tendon. If it’s your rotator cuff, you’ll feel it when you reach overhead. If it’s your Achilles, you’ll feel a sharp sting when you push off to walk or run.
Here’s the kicker: 65% of shoulder pain cases involve both bursitis and tendinitis happening at the same time. That’s why so many people get confused. You think it’s a torn rotator cuff, but it’s really the bursa rubbing against an inflamed tendon. And if you treat it like a tendon problem when it’s mostly bursitis, you might end up doing exercises that make the swelling worse.
How Do Doctors Know Which One You Have?
There’s no single blood test or X-ray that tells you definitively. Diagnosis comes from three things: where the pain is, what makes it worse, and how it feels when pressed.
For bursitis, doctors press on the swollen area. If it’s tender and feels squishy, like a water balloon under the skin, it’s likely the bursa. Pain gets worse when you lie on it or press directly on it. Movement might hurt, but it’s not always tied to a specific motion.
For tendinitis, the pain is more like a tug-of-war. It flares up during specific movements - lifting your arm, bending your wrist, pushing off your toes. If you do the same motion slowly and it hurts more as you go through the range, that’s a classic sign. A test called the “painful arc” - where shoulder pain happens between 60 and 120 degrees of lifting - is often used for rotator cuff tendinitis.
Ultrasound is now the go-to tool for confirmation. It’s accurate in 92% of cases, shows swelling in real time, and doesn’t cost a fortune. MRI can show more detail, but it’s overkill for most cases. Many people get MRIs and see "tendinitis" on the scan - even if they have no pain. One study found that 40% of people over 50 have signs of tendinitis or bursitis on MRI with zero symptoms. So don’t trust a scan alone. Your symptoms matter more.
Why Misdiagnosis Makes Recovery Take Longer
Getting the wrong diagnosis isn’t just frustrating - it’s costly. A 2023 study tracked 1,520 patients who were initially treated for the wrong condition. Those with misdiagnosed bursitis were given strengthening exercises too early. Those with tendinitis were given cortisone shots when they didn’t need them. The result? Their pain lasted 3.2 times longer than those who got the right treatment from the start.
Here’s a real example: Sarah, 52, a retired teacher, started having elbow pain after gardening. She thought it was "tennis elbow" - a common tendinitis. She did wrist stretches, used a brace, and waited. Six weeks later, nothing changed. She went to a specialist, who found her bursa was swollen, not her tendon. She got one cortisone injection. Within ten days, her pain dropped by 80%. She’d wasted two months because the pain was in the right spot, but the cause wasn’t what she assumed.
Another trap: cortisone shots. They work great for bursitis - 78% of patients report big relief within four weeks. But for tendinitis? Only 52% benefit. Worse, injecting cortisone directly into a tendon can weaken it over time. That’s why experts warn: never inject a tendon unless you’re absolutely sure it’s the problem.

What Actually Works to Fix These Problems
The good news? Most cases get better without surgery. In fact, fewer than 5% of people ever need an operation.
Step one: Stop doing what hurts. Not completely - just enough to let the inflammation calm down. If your shoulder hurts when you reach for a high shelf, don’t stop using your arm. Just avoid lifting things over your head for a week or two. Rest doesn’t mean lying still. It means changing how you move.
Ice helps - especially in the first few days. Use a frozen water bottle and roll it over the sore spot for 10 minutes, twice a day. It’s cheaper than a gel pack and works just as well. One survey of 189 people found ice massage rated 4.2 out of 5 for effectiveness.
NSAIDs like ibuprofen or naproxen can help with pain and swelling, but don’t take them longer than 10-14 days. Long-term use can hurt your stomach or kidneys. If you need pain relief beyond that, talk to your doctor about alternatives.
For bursitis, once the sharp pain fades, gentle movement is key. Slow shoulder circles, elbow bends - anything that keeps the joint moving without pressure. Avoid lying on the sore side. Use a pillow to cushion it at night.
For tendinitis, the real game-changer is eccentric strengthening. This sounds fancy, but it’s simple: slowly lowering a weight after lifting it. For Achilles tendinitis, that means standing on your toes on a step, then slowly lowering your heel down over 3-5 seconds. Do 3 sets of 15 reps, twice a day. That’s 90 reps. For 12 weeks. It’s boring. It’s hard. But it works better than any shot or pill. One study showed 68% of people with chronic Achilles tendinitis had lasting improvement after this program, compared to just 41% who got injections.
When to See a Doctor - and What to Ask
You don’t need to rush to the ER for this. But if pain lasts more than two weeks despite rest and ice, or if you can’t move the joint at all, it’s time to see someone.
When you go, don’t just say, "My shoulder hurts." Say: "It hurts when I lift my arm overhead, especially above shoulder height. It’s worse at night when I lie on it. I’ve tried ice and ibuprofen for two weeks with no change. I’m worried it might be bursitis or a tendon issue. Can we check with an ultrasound?"
Ask about activity modification. Ask what movements to avoid. Ask if a cortisone shot is appropriate - and if so, which structure it’s being injected into. And ask for a referral to a physical therapist who specializes in joint problems. Certified hand therapists or sports PTs know exactly which exercises help which condition.
What to Avoid - Even If It’s Popular
There’s a lot of bad advice out there.
- Don’t stretch a painful tendon. Stretching inflamed tissue can make it worse. Focus on slow, controlled strengthening instead.
- Don’t use a brace all day. Braces can help short-term, but wearing them too long weakens the muscles around the joint.
- Don’t ignore pain that gets worse during exercise. If you feel pain above a 3 out of 10 while moving, stop. You’re not "working through it" - you’re causing more damage.
- Don’t believe the myth that "more pain equals more progress." That’s not true. Progress is measured by less pain over time, not more strain.
Also, avoid PRP (platelet-rich plasma) or shockwave therapy unless you’ve tried everything else. They’re expensive - PRP costs around $850 per injection - and while they show promise for chronic cases, they’re not first-line treatments. Stick with proven, low-cost methods first.
Real People, Real Recovery
Tom Wilcox, a former runner from Australia, had chronic Achilles tendinitis for 18 months. He tried rest, braces, massage, even acupuncture. Nothing stuck. Then he found the Alfredson protocol: 180 eccentric heel drops a day, split into three sets. He did it for 12 weeks. No painkillers. No shots. Just slow, painful, consistent movement. He tracked his progress with a simple questionnaire. At week 12, his pain dropped from 8/10 to 1/10. He’s been running again for two years.
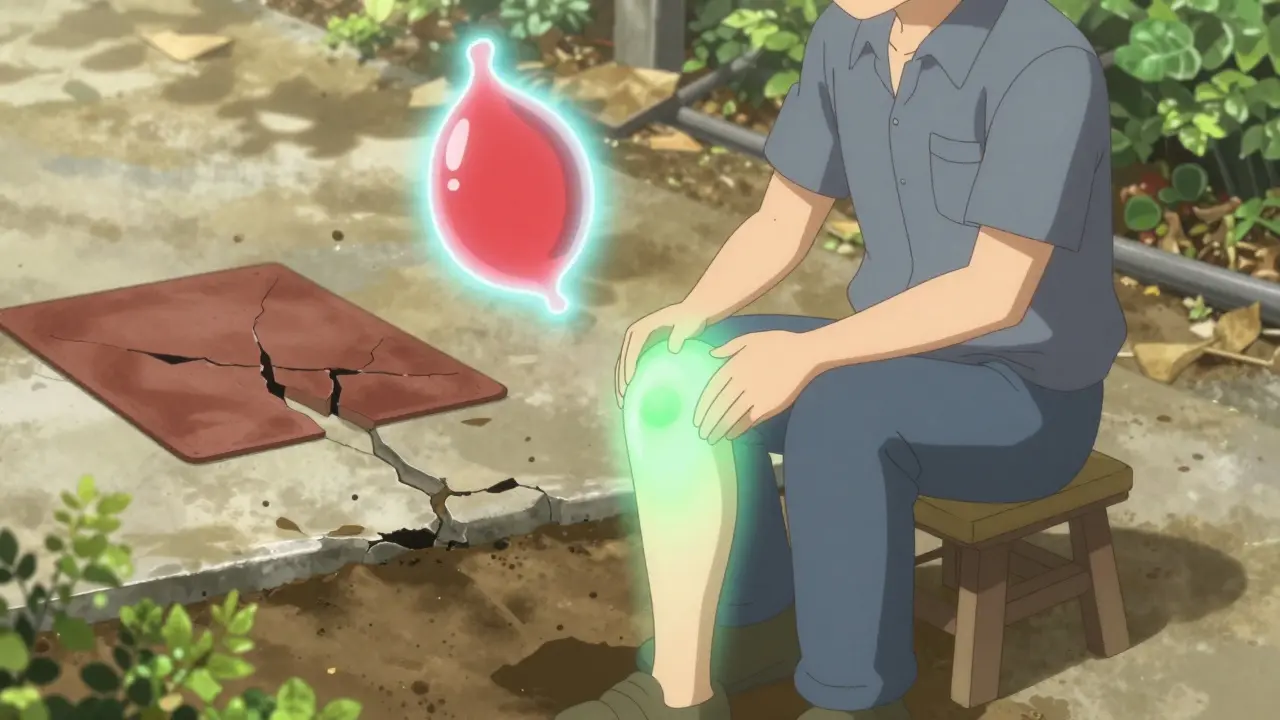
On Reddit, a construction worker shared how he fixed his knee bursitis by switching from kneeling pads to a small stool. He’d been kneeling for hours on concrete. The bursa was crushed. Once he stopped putting direct pressure on it, the swelling went down in three weeks. He didn’t need a shot. He just changed his tool.
These aren’t magic fixes. They’re smart ones. The common thread? Patience. Precision. And listening to your body - not the internet.
Prevention: Stop It Before It Starts
These conditions don’t come out of nowhere. They’re the result of repeated stress. So prevention is about reducing that stress.
- If you work at a desk, adjust your chair and monitor so you don’t hunch your shoulders.
- If you garden, use knee pads or a stool - don’t kneel on concrete.
- If you play tennis or lift weights, warm up properly. Don’t skip mobility work.
- Strengthen the muscles around your joints. Stronger muscles take pressure off tendons and bursae.
- Listen to early warning signs. A twinge after yoga? A dull ache after walking? Don’t ignore it. Rest for a day. Ice it. See if it comes back.
The best time to fix this is before it becomes a problem. Most people wait until they can’t sleep, can’t lift their coffee cup, or can’t walk without limping. Don’t wait that long.
Can bursitis and tendinitis happen at the same time?
Yes, very commonly. In fact, about 65% of shoulder pain cases involve both the bursa and the rotator cuff tendon being irritated at once. This is why misdiagnosis is so common - treating just one part may not fix the whole problem. A good doctor will check both structures and adjust treatment accordingly.
Is cortisone safe for tendinitis?
It’s risky. Cortisone shots work well for bursitis, but injecting them directly into a tendon can weaken it and increase the chance of a tear. Experts recommend avoiding tendon injections unless the pain is severe and hasn’t improved with 6-8 weeks of physical therapy. Even then, no more than two or three shots per year.
How long does it take to recover from tendinitis?
Tendinitis takes longer than bursitis. Bursitis often improves in 4-6 weeks with rest and anti-inflammatories. Tendinitis usually needs 12-16 weeks of targeted strengthening exercises to fully heal. Rushing back to activity too soon is the #1 reason it comes back.
Should I use a brace for bursitis or tendinitis?
A brace can help short-term by reducing movement and giving the area a break. But wearing it all day weakens the muscles and can make the problem worse over time. Use it only for 1-2 weeks during flare-ups, then start gentle movement. Long-term recovery depends on strength, not support.
Can I still exercise with bursitis or tendinitis?
Yes - but you need to modify it. Avoid the movement that causes pain. If your shoulder hurts when you press weights overhead, switch to seated rows or light dumbbell flies. Stay active, but stay smart. Pain above a 3 out of 10 during exercise means you’re pushing too hard. Use the "pain monitoring rule" - keep discomfort low and consistent.
Is tendinitis the same as tendinopathy?
The term "tendinitis" implies active inflammation, but many chronic cases aren’t inflamed at all - they’re degenerated. That’s why experts now prefer "tendinopathy" for long-term cases. The treatment is the same: eccentric strengthening, not anti-inflammatories. But understanding this shift helps explain why rest and ice don’t always work - you’re not treating inflammation, you’re rebuilding tissue.
Final Thought: It’s Not Just Pain - It’s a Message
Your body isn’t broken. It’s telling you something. The pain in your elbow isn’t random. It’s the result of how you move, how you work, how you rest. Fixing bursitis or tendinitis isn’t about finding the magic pill or shot. It’s about listening - to your body, to your doctor, and to the slow, steady progress that comes from smart, consistent care. You don’t need to stop living. You just need to move smarter.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.