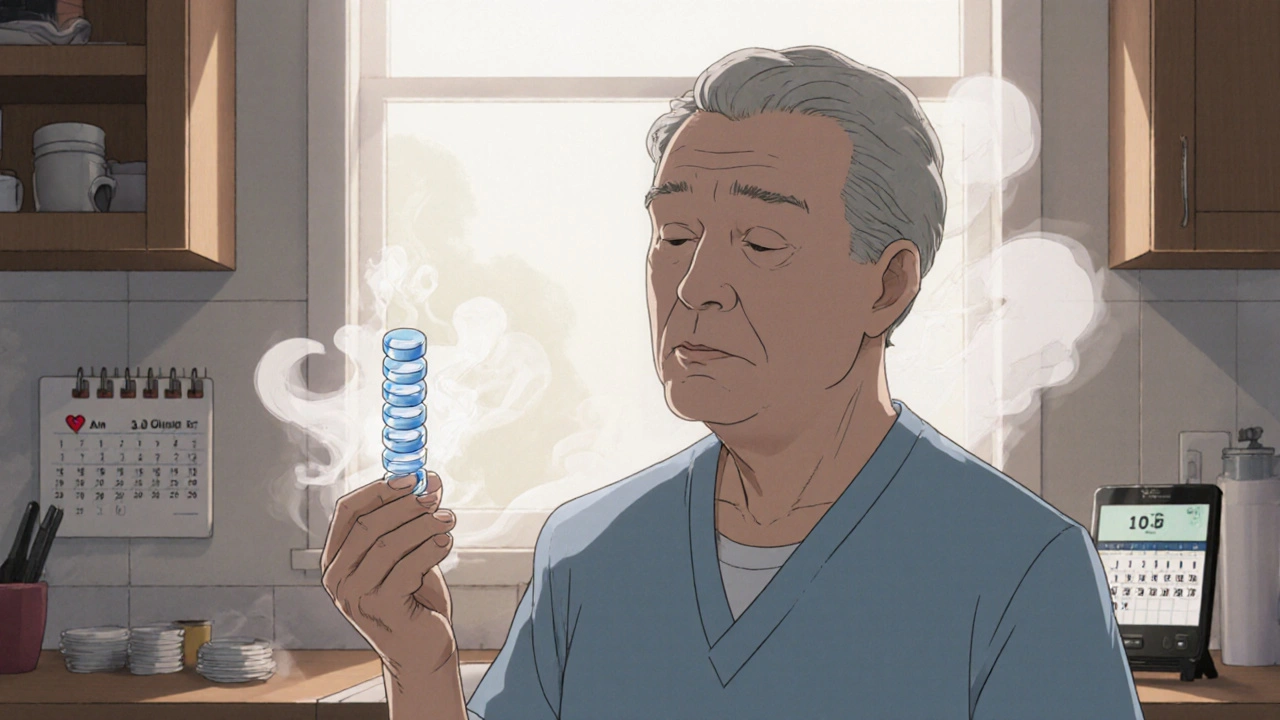
When you’re managing heart disease, diabetes, or high blood pressure, taking multiple pills every day isn’t just inconvenient-it’s a major reason why people stop taking their meds. Studies show that when patients have to take four or more separate pills daily, adherence drops to just 25-30%. But what if you could take just one pill instead? That’s the promise of cardiovascular combination generics: single pills that combine two or more heart medications into one dose. They’re not new, but they’re becoming more common-and more important-than ever.
What Are Cardiovascular Combination Generics?
These are generic versions of fixed-dose combination drugs that bundle two or more cardiovascular medications into a single tablet. Common combinations include:
- ACE inhibitor + diuretic (e.g., lisinopril + hydrochlorothiazide)
- Statins + ezetimibe (e.g., simvastatin + ezetimibe)
- Calcium channel blocker + ACE inhibitor (e.g., amlodipine + benazepril)
- Angiotensin receptor blocker + diuretic (e.g., losartan + hydrochlorothiazide)
- Antiplatelet + statin (e.g., aspirin + atorvastatin-less common in the U.S.)
The goal? Reduce pill burden, cut costs, and boost adherence. The science backs it up: patients on combination pills are 15-20% more likely to stick with their treatment than those taking the same drugs separately. That’s not a small gain-it’s the difference between preventing a heart attack and ending up in the hospital.
Why These Combinations Work Better
Think of your heart meds like a team. Each drug has a job: one lowers blood pressure, another reduces cholesterol, another prevents clots. But when you have to take them at different times, with different food rules, and in different pill forms, it’s easy to forget one-or all.
A 2017 Medicare analysis found that 43.8% of cardiovascular prescriptions were still for brand-name drugs-even though generics were available. That’s over $1.3 billion a year in avoidable spending. Generic combination pills typically cost 80-85% less than their brand-name counterparts. For example, a 30-day supply of brand-name Vytorin (ezetimibe/simvastatin) used to run over $200. The generic? Around $15.
But cost isn’t the only win. A 2020 study in Circulation: Cardiovascular Quality and Outcomes showed that patients on single-pill combinations had adherence rates of 75-85%, compared to 50-60% for multiple separate pills. That’s not magic-it’s simplicity. One pill. One time a day. Less room for error.
Commonly Available Generic Combinations
Not all combinations are available as generics. But many are. Here’s what you’re likely to find in U.S. pharmacies today:
| Combination | Brand Name (Discontinued or Limited) | Generic Availability | Typical Cost (30-day supply) |
|---|---|---|---|
| Lisinopril + Hydrochlorothiazide | Zestoretic | Yes (since 2007) | $10-$18 |
| Amlodipine + Lisinopril | Lotrel | Yes (since 2015) | $12-$20 |
| Simvastatin + Ezetimibe | Vytorin | Yes (since 2016) | $15-$25 |
| Losartan + Hydrochlorothiazide | Hyzaar | Yes (since 2014) | $10-$16 |
| Atorvastatin + Amlodipine | Caduet | Yes (since 2018) | $18-$30 |
| Carvedilol + Hydrochlorothiazide | Coreg HCT | No (brand discontinued) | Take separately |
Notice the gap? Carvedilol + hydrochlorothiazide never had a generic combo, even though both components are cheap generics. That means patients still take two pills. Same with metoprolol + hydrochlorothiazide-no combo version exists in the U.S. So while many options are available, not every logical combo is on the shelf.
What About the "Polypill"?
The dream? A single pill with aspirin, a statin, an ACE inhibitor, and a beta-blocker. That’s the "polypill"-a concept first proposed in 2002 by Dr. Salim Yusuf. He estimated it could cut heart attack and stroke risk by 75% in high-risk patients.
Here’s the catch: while each of those four drugs is available as a generic in the U.S., no single pill combines all four. Some countries-like India and parts of Europe-have polypills in routine use. In Australia, the government even subsidizes a version for patients after a heart attack. But in the U.S., regulatory hurdles and lack of commercial interest have stalled progress.
Why? Drug companies don’t make much profit on generics. And no single manufacturer has pushed for a four-drug combo because it’s hard to patent, and there’s little incentive to invest in development. So for now, the polypill remains a promising idea-not a reality-for most Americans.
Are Generic Combos Safe? The Evidence
People worry: "Will the generic work the same?" The answer, based on decades of data, is yes.
The FDA requires generic drugs to be bioequivalent to brand-name versions. That means they deliver 80-125% of the active ingredient into your bloodstream at the same rate. For most heart meds, that’s more than enough. A 2014 European Heart Journal review of 61 clinical trials found no meaningful difference in safety or effectiveness between brand and generic cardiovascular drugs.
There’s one exception: drugs with a narrow therapeutic index-like warfarin. Small changes in blood levels can be dangerous. That’s why some doctors still prefer brand-name warfarin, even though generic versions are approved. But for statins, beta-blockers, ACE inhibitors, and calcium channel blockers? The data is clear: generics work just as well.
A 2019 survey of 1,245 patients on Drugs.com found that 78% said generic heart meds were "equally effective" as brand-name versions. Only 12% reported side effects they blamed on the generic. Pharmacists, who see this daily, report that 89% of their patients accept generics after a quick explanation.
When You Should Be Cautious
Not every switch is safe. Here are three red flags:
- You’re on a medication with a narrow therapeutic window. Warfarin, digoxin, and some anti-seizure drugs need extra monitoring. Switching generics here requires blood tests.
- You’ve had side effects with a specific brand. Some people report differences in inactive ingredients-like dyes or fillers-that can cause bloating, rashes, or stomach upset. If you notice new symptoms after switching, tell your doctor.
- You’re in a state with strict substitution rules. In 18 states, pharmacists must get your consent before swapping a brand for a generic. In others, substitution is automatic. Know your rights.
Also, don’t assume a combo pill is always better than two separate generics. Sometimes, mixing two generics yourself gives you more flexibility to adjust doses. For example, if your blood pressure drops too low on amlodipine + lisinopril, you can’t easily lower the dose of just one component. With separate pills, you can tweak each one independently.
What’s New in 2025?
The landscape is shifting. In 2022, the first generic version of Entresto (sacubitril/valsartan) hit the market. That’s a big deal-it’s a life-changing drug for heart failure patients, and now it’s affordable.
The FDA also released new draft guidance in 2021 to speed up approval of fixed-dose combinations. That means more combos could be on the way. Experts are pushing for a U.S. polypill for post-heart attack patients. The World Heart Federation estimates that if polypills were widely adopted in low- and middle-income countries, they could prevent 15-20 million cardiovascular deaths over the next decade.
In the U.S., adoption is still slow. A 2018 study found only 45% of primary care doctors knew all the available generic combos. That’s changing, but slowly. More prescribers are starting to ask: "Is there a combo version?" instead of defaulting to separate pills.
What You Can Do Right Now
If you’re on multiple heart meds, here’s your action plan:
- Ask your pharmacist: "Are any of my medications available as a combination pill?" They have access to databases that list all available combos.
- Ask your doctor: "Could I switch to a single-pill combo?" Don’t assume they know all the options-many don’t.
- Check your copay. If you’re paying $50+ for two separate pills, a combo might cost $15. Ask for a price comparison.
- If you’ve had side effects after switching to a generic, don’t assume it’s "all generics." Report it. It might be a specific manufacturer’s version.
- Don’t stop or switch meds on your own. Always talk to your provider first.
The bottom line? Cardiovascular combination generics aren’t a miracle. But they’re one of the most practical, cost-effective tools we have to keep people alive and out of the hospital. They’re not perfect. But they’re better than taking five pills a day-and far cheaper than a heart attack.
Frequently Asked Questions
Are cardiovascular combination generics as effective as brand-name drugs?
Yes. The FDA requires generic combination drugs to be bioequivalent to brand-name versions, meaning they deliver the same amount of active ingredient into your bloodstream within an acceptable range. Multiple studies, including a 2014 review of 61 clinical trials in the European Heart Journal, show no significant difference in effectiveness or safety for common heart medications like statins, ACE inhibitors, and beta-blockers.
Why isn’t there a "polypill" with aspirin, statin, ACE inhibitor, and beta-blocker in the U.S.?
Each of those four drugs is available as a generic, but no single pill combines all four in the U.S. The main reason is lack of commercial incentive. Generic manufacturers don’t profit much from new combinations, and there’s no patent protection to justify the development cost. Some countries like India and Australia use polypills routinely, but U.S. regulators and insurers haven’t prioritized them yet.
Can I switch from brand-name heart meds to generics on my own?
No. Never switch medications without talking to your doctor. Even though generics are generally safe, your doctor needs to approve the change and monitor you for side effects. In 18 states, pharmacists must get your consent before substituting a brand for a generic. In others, substitution happens automatically-so make sure you know what’s happening with your prescriptions.
Why do some people say generics make them feel worse?
It’s usually not the active drug-it’s the inactive ingredients. Fillers, dyes, or coatings can vary between brands and generics. Some people report bloating, rashes, or stomach upset after switching. These reactions are rare, but real. If you notice new symptoms after switching, tell your doctor. You may need to try a different generic manufacturer or go back to the brand.
How much money can I save with combination generics?
Significantly. In 2017, Medicare data showed brand-name cardiovascular drugs cost an average of $85.43 per fill, while generics averaged $15.67. A combination pill can cut your monthly cost by 70-80%. For example, if you’re paying $120 for two separate pills, switching to a generic combo could drop your bill to $20 or less-sometimes even under $10 with discount programs.
Is it better to take two separate generics or one combo pill?
It depends. A combo pill improves adherence and simplifies your routine. But if your doses need to be adjusted frequently-say, your blood pressure fluctuates-a combo might be too rigid. With separate pills, you can increase or decrease one component without changing the other. Talk to your doctor about what fits your lifestyle and medical needs.
Next Steps
If you’re on multiple heart medications, schedule a med review with your doctor or pharmacist. Bring a list of everything you take-prescription, over-the-counter, supplements. Ask: "Is there a combination generic that could replace two or more of these?" If your current combo isn’t available as a generic, ask if splitting the dose into separate generics would save money and still work.
Also, check your pharmacy’s discount programs. Many offer $4 generics-even for combo pills. You’d be surprised how often the cash price is lower than your insurance copay.
Cardiovascular combination generics aren’t the future. They’re the present. And for millions of people, they’re the simplest, cheapest way to stay healthy.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.