Skipping a pill here and there might seem harmless. Maybe you forgot. Maybe you felt fine. Maybe the cost was too high. But when you don’t take your medication exactly as your doctor ordered, the consequences aren’t just minor-they can be life-altering, even deadly.
Every Missed Dose Adds Up
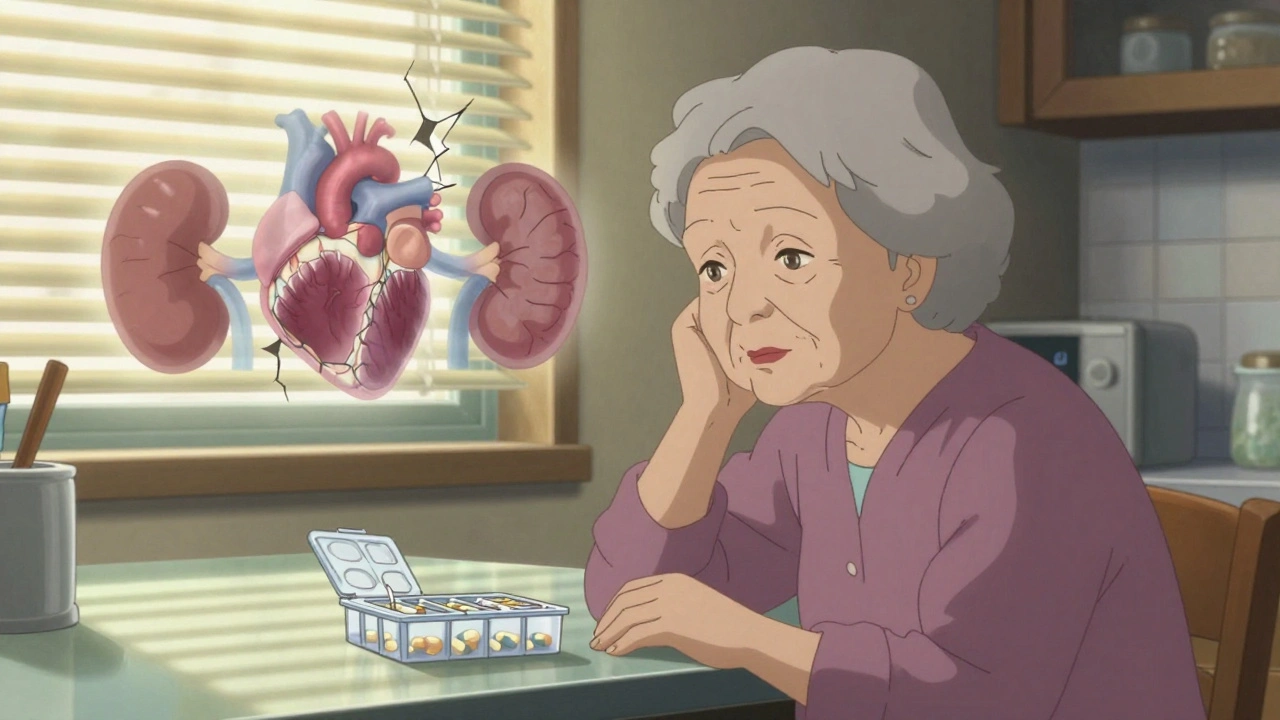
Medications for chronic conditions like high blood pressure, diabetes, or depression aren’t meant to be taken only when you feel like it. They work by keeping a steady level of the drug in your body. Skip a dose, and that level drops. Take it late, and the rhythm breaks. Over time, this inconsistency doesn’t just reduce effectiveness-it can make your condition worse.For example, if you have high blood pressure and skip your pills, your arteries stay under stress. That stress doesn’t disappear just because you feel okay. It silently damages your heart, kidneys, and brain. Studies show that people who don’t take their blood pressure meds as directed are three times more likely to have a stroke. The same pattern holds for diabetes: skipping insulin or oral meds leads to higher blood sugar, nerve damage, and increased risk of amputation.
Even in mental health, skipping doses can trigger a cascade. People with depression or bipolar disorder who miss pills are far more likely to relapse, end up in the ER, or attempt suicide. One study found that nearly 60% of people with serious mental illness inconsistently take their meds. That’s not laziness-it’s often fear of side effects, stigma, or not understanding how the drug works.
The Cost of Skipping Isn’t Just Financial
It’s easy to think, “I’ll just skip today because I can’t afford it.” But skipping doesn’t save money-it costs more in the long run. The U.S. spends between $100 billion and $300 billion every year treating problems caused by people not taking their meds. That’s not hypothetical. That’s hospital stays, emergency visits, and long-term disability.One in five Medicare patients who get readmitted within 30 days are sent back because they didn’t take their meds. And half of those readmissions? Directly tied to nonadherence. That’s not bad luck. That’s preventable. The average cost of one hospitalization due to missed pills? Between $5,000 and $50,000 per person. Compare that to the $10 you pay for a 30-day supply of your blood thinner. The math doesn’t add up.
And it’s worse for older adults. Up to 100,000 deaths each year in the U.S. among seniors are linked to not taking medications properly. That’s more than traffic accidents. More than opioid overdoses. And most of those deaths could have been avoided with simple support.
Why Do People Skip?
It’s not about being irresponsible. Most people who miss doses have real, valid reasons.Cost is the biggest barrier. In 2021, 8.2% of working-age adults in the U.S. said they didn’t take their meds because they couldn’t afford them. That number is rising. Out-of-pocket drug costs jumped nearly 5% in just one year. For someone on a fixed income, choosing between insulin and groceries isn’t a choice-it’s a crisis.
Complex regimens are another killer. If you’re on five different pills, each with different times, food rules, and side effects, it’s easy to get lost. One study found that people taking four or more daily medications are twice as likely to miss doses. That’s why pill organizers and once-daily formulations help so much.
Fear of side effects is huge. People stop their statins because they’re scared of muscle pain. They quit antidepressants because they feel “numb.” But they don’t tell their doctor. They just stop. And that silence is dangerous. Most side effects are temporary or manageable-if you talk to your provider. But silence? That’s how bad outcomes happen.
Lack of understanding is often overlooked. Many patients don’t know why they’re on a drug. They think, “I don’t have symptoms, so I don’t need it.” That’s true for painkillers-but not for blood pressure, cholesterol, or thyroid meds. Those drugs work behind the scenes. You won’t feel better. But you’ll stay alive.

Who’s Most at Risk?
This isn’t an equal-opportunity problem. Minority communities-Black, Latino, Indigenous, and low-income groups-face higher rates of nonadherence. Why? Because of systemic gaps: fewer pharmacies nearby, language barriers, mistrust from historical mistreatment in healthcare, and lack of culturally competent care.Older adults are also at higher risk. Memory issues, vision problems, and multiple doctors prescribing different meds make adherence harder. A 75-year-old with heart disease, diabetes, and arthritis might be taking 12 pills a day. No wonder they mix them up.
And then there’s mental health. People with depression often lack the energy to manage their meds. Anxiety makes them fear side effects. Trauma makes them distrust doctors. These aren’t personality flaws-they’re symptoms of illness. And they need support, not judgment.
What Actually Works to Fix This
There’s no magic fix. But there are proven solutions.Pharmacist-led programs have boosted adherence by 15-20%. Pharmacists aren’t just pill dispensers. They’re trained to review your entire regimen, spot conflicts, simplify schedules, and answer questions you’re too shy to ask your doctor.
Text reminders work. Simple, daily texts saying “Take your lisinopril” have improved adherence by 12-18% in trials. No apps. No subscriptions. Just a text.
Pill organizers with alarms? Game-changers. Especially for older adults. A simple weekly box with morning and night compartments cuts confusion.
Medication therapy management (MTM) programs-where a pharmacist spends 20-30 minutes with you monthly to review your meds-save money. For every $1 spent on MTM, healthcare systems save $3 to $10 in avoided hospital visits.
But here’s the catch: most of these services aren’t covered by insurance. Pharmacies don’t get paid to help you take your pills. Doctors don’t get reimbursed for talking about adherence. So they don’t do it.

What You Can Do Today
You don’t need a perfect system. You need a simple one.- Ask your doctor: “Can I take this once a day instead of twice?” or “Is there a cheaper version?”
- Ask your pharmacist: “Can you put my meds in a weekly organizer?” They’ll do it for free.
- Set a daily phone alarm: Label it with the drug name. Don’t just say “Meds.” Say “Blood pressure pill.”
- Don’t stop cold turkey: If you’re scared of side effects, call your doctor. Don’t quit. They can adjust the dose or switch you.
- Use a pill box: Even a cheap one from the dollar store helps. Fill it every Sunday.
If you’re skipping meds because of cost, ask about patient assistance programs. Most drug makers offer free or low-cost versions if you qualify. Pharmacies like CVS and Walgreens have discount lists for common meds. You don’t have to pay full price.
The Bigger Picture
This isn’t just about you. It’s about your family, your community, and the healthcare system. When you skip your meds, you increase the risk of hospitalization. That means longer wait times for others. Higher insurance premiums for everyone. More strain on nurses and doctors who are already burned out.And it’s personal. Every time you take your pill, you’re choosing to protect your future self. The version of you who wants to walk with your grandkids. Who wants to travel. Who doesn’t want to be stuck in a hospital bed because a simple habit was ignored.
Medication adherence isn’t about obedience. It’s about empowerment. It’s about knowing your body, trusting your care team, and taking back control-one pill at a time.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.