Most people think a runny nose and sore throat mean the same thing - a cold. But if you wake up feeling like you’ve been hit by a truck, with a fever, body aches, and exhaustion so deep you can’t get out of bed, that’s not a cold. That’s the flu. And confusing the two can cost you time, health, and even money.
How to Tell a Cold From the Flu
The common cold and influenza start with similar symptoms: cough, sore throat, congestion. But that’s where the similarity ends. A cold creeps in. You might feel a little scratchy in your throat on Monday, sneeze a bit Tuesday, and by Wednesday you’re blowing your nose nonstop. Fever? Rare in adults - only about 1 in 5 people with a cold get one, and it’s usually mild, under 100°F.
Flu hits like a siren. One moment you’re fine. The next, you’re shivering, achy, and burning up. Fever hits fast - often above 102°F - and stays for 3-4 days. Headaches? Common. Muscle pain? Severe. Fatigue? So bad it lasts weeks. You won’t just feel tired - you’ll feel hollowed out. That kind of exhaustion doesn’t happen with a cold.
Doctors use a simple rule: if your symptoms came on suddenly and you’re too weak to stand, assume it’s flu until proven otherwise. Cold symptoms build slowly over 2-3 days. Flu symptoms appear in under 24 hours.
Why Misdiagnosis Costs More Than Time
Every year, about 30% of antibiotic prescriptions in the U.S. are given for viral infections like colds and flu. That’s not just wrong - it’s dangerous. Antibiotics don’t kill viruses. They kill good bacteria, trigger side effects like diarrhea and yeast infections, and help create superbugs that no drug can touch.
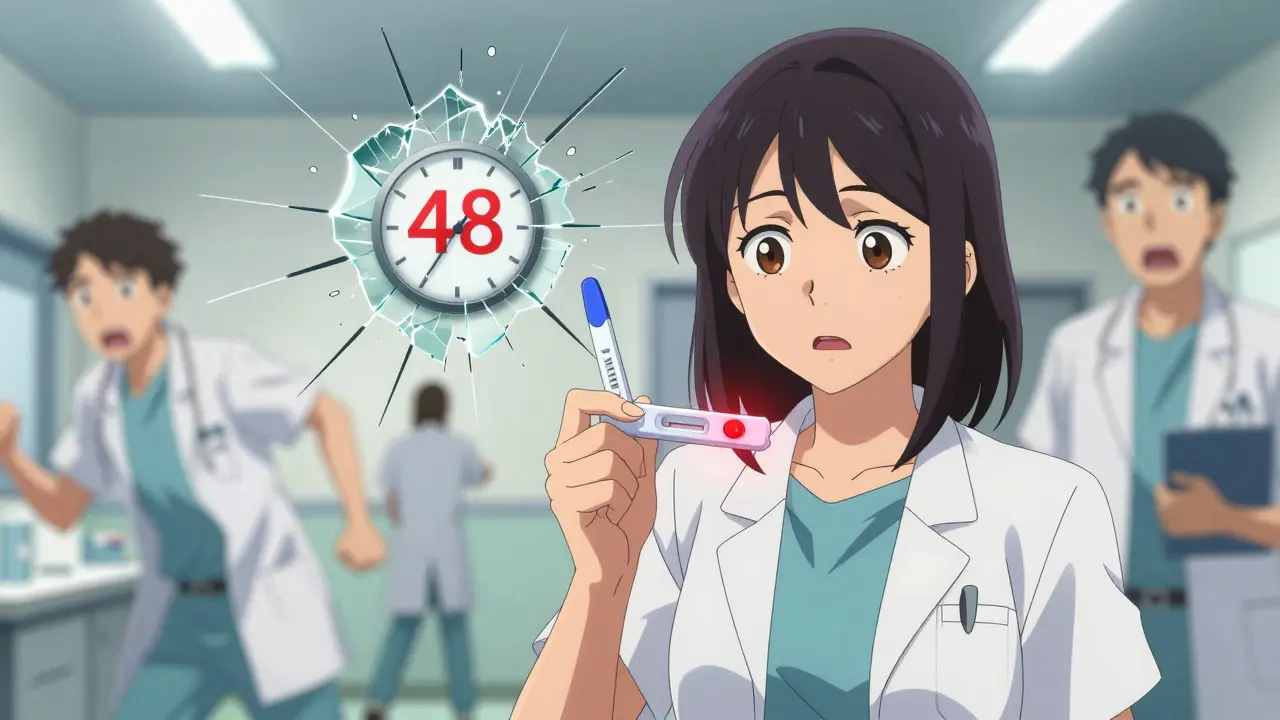
But the bigger risk is missing flu when it’s still treatable. Antivirals like oseltamivir (Tamiflu) and baloxavir (Xofluza) can cut your illness short by 1-2 days - if you take them within 48 hours of the first symptom. After that? They barely help. Yet studies show only 18% of high-risk patients get antivirals on time. Why? Because they think it’s just a bad cold.
Real people tell the same story on Reddit and patient forums: “I waited three days because I thought it was a cold. By day five, I was in the ER with pneumonia.” That’s not rare. It’s predictable.
Complications: When a Cold Becomes Dangerous
Colds rarely turn serious. About 5% of adults develop sinus infections. Kids might get ear infections. That’s it. Most recover without seeing a doctor.
Flu? It’s a different story. Each year in the U.S., flu leads to 140,000 to 710,000 hospitalizations. About 1 in 5 people hospitalized with flu develop pneumonia - sometimes bacterial, sometimes viral. That’s when oxygen levels drop, breathing gets hard, and you need IV fluids and antibiotics. In 2022-2023, flu sent more than 30,000 people under 65 into the hospital. That’s not just seniors - it’s young parents, teachers, delivery drivers.
High-risk groups include anyone over 65 (they make up 80% of flu deaths), pregnant women (three times more likely to be hospitalized), and people with asthma, diabetes, or weakened immune systems. If you’re in one of these groups and feel flu symptoms, don’t wait. Call your doctor the same day.
Antivirals: What Actually Works - and What Doesn’t
There are four FDA-approved antivirals for flu: oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), and baloxavir (Xofluza). All work by blocking the virus from spreading in your body. None work on colds. Not one.
Oseltamivir is the most common. Generic versions cost $15-$30 for a 5-day course. Brand-name Tamiflu? Around $150 without insurance. It cuts symptom duration by about 30 hours on average. Side effects? Nausea in about 10% of users - but it’s usually mild.
Baloxavir (Xofluza) is newer. One pill. Works in 24 hours. Reduces viral load by 99%. But it costs $150-$200. For a healthy 30-year-old with mild flu? Maybe not worth it. For a 70-year-old with COPD? Absolutely. Insurance often covers it for high-risk patients.
Here’s the catch: timing is everything. If you wait 72 hours, antivirals lose most of their power. That’s why urgent care centers now offer rapid flu tests - results in 15 minutes. If you’re sick and high-risk, get tested. Don’t guess.
And no - zinc lozenges, vitamin C, echinacea, and garlic won’t stop the flu. Some studies show zinc *might* shorten a cold by 1.6 days if taken within 24 hours. But the metallic taste makes most people quit after day one. And it doesn’t touch flu.
What About the Flu Shot?
The flu vaccine isn’t perfect. In 2022-2023, it was about 50% effective. That means half the people who got vaccinated still got sick. But here’s the thing: vaccinated people who got flu had 40% fewer hospitalizations and 30% less severe symptoms.
The 2023-2024 vaccine covers four strains: two A strains (H1N1 and H3N2) and two B strains. It’s updated every year because flu viruses change fast. The new mRNA flu vaccines (like Moderna’s mRNA-1010) are in late-stage trials and could be available by 2025. They’re designed to trigger a stronger, longer-lasting immune response.
But vaccines take weeks to work. If you’re already sick, the shot won’t help. It’s for next season - not this one.
When to Worry: Emergency Signs
Most colds and flus get better on their own. But some symptoms mean you need help right now:
- Difficulty breathing or shortness of breath
- Chest pain or pressure
- Confusion or dizziness
- Severe vomiting or inability to keep fluids down
- Bluish lips or face
If you or someone you care about has any of these, go to the ER. Don’t wait. Don’t call your doctor. Go.

What to Do Right Now
If you’re sick today:
- Check your symptoms. Did they hit suddenly? Fever over 101°F? Body aches? That’s flu territory.
- If you’re over 65, pregnant, or have a chronic illness - call your doctor today. Ask for a flu test and antiviral.
- If you’re young and healthy, rest, hydrate, and take acetaminophen for fever. Avoid ibuprofen if you’re dehydrated.
- Don’t take antibiotics. They won’t help and might hurt you later.
- Stay home for at least 24 hours after your fever breaks. You’re still contagious.
If you’re not sick yet:
- Get your flu shot if you haven’t. It’s still January - flu season runs through March.
- Wash your hands. Flu spreads through droplets - not just coughs, but handshakes, doorknobs, keyboards.
- Keep a thermometer and fever reducer at home. Don’t wait until you’re too sick to think clearly.
Common Myths, Debunked
- Myth: Cold weather causes colds. Truth: Viruses cause colds. You’re more likely to get sick indoors in winter because people are packed together.
- Myth: Flu shots give you the flu. Truth: The vaccine contains dead virus. You might feel sore or tired for a day - but you won’t get flu from the shot.
- Myth: Antivirals are for everyone. Truth: They’re most helpful for high-risk people. For healthy adults, the benefit is small - but still real if taken early.
- Myth: If you had the flu last year, you’re immune. Truth: Flu changes every year. Last year’s strain won’t protect you this year.
What’s Next for Flu Treatment?
Scientists are working on a universal flu vaccine - one that works against all strains, not just the ones predicted for the season. Early trials in animals show 70% protection across multiple strains. Human trials are underway. If it works, we could stop chasing new vaccines every fall.
Meanwhile, antivirals are getting smarter. New drugs in development target the virus’s replication machinery differently, making resistance less likely. Right now, about 1.5% of H1N1 strains are resistant to oseltamivir. That number could rise if we keep delaying treatment.
Climate change is making things harder too. Flu seasons are now 12 days longer than they were in 2000. Warmer winters mean viruses survive longer outside the body. More people are traveling. More strains are mixing.
But here’s the good news: we know what works. Antivirals save lives when used early. Vaccines reduce severity. Handwashing stops spread. Simple things. But only if we act fast - and don’t mistake a fever for a cold.”
Can you get the flu from the flu shot?
No. The flu vaccine contains inactivated (dead) virus or just a piece of the virus - it can’t cause infection. Some people feel mild side effects like soreness, low-grade fever, or fatigue for a day or two, but that’s your immune system responding, not the flu itself.
How long am I contagious with the flu?
You can spread flu one day before symptoms start and up to 5-7 days after. Kids and people with weak immune systems can be contagious for even longer. Stay home until you’ve been fever-free for at least 24 hours without fever-reducing meds.
Do antivirals work against colds?
No. Antivirals like Tamiflu and Xofluza only target influenza viruses. Colds are caused by over 200 different viruses - mostly rhinoviruses - and there are no approved antivirals for them. Treatment is limited to rest, fluids, and symptom relief.
Is it safe to take zinc for a cold?
Zinc lozenges may shorten a cold by about 1.6 days if taken within 24 hours of symptoms - but many people can’t tolerate the metallic taste. Long-term use can cause copper deficiency and loss of smell. The CDC says evidence is inconsistent, so it’s not a recommended treatment.
Should I get tested for flu if I’m healthy?
If you’re young and healthy with mild symptoms, testing isn’t usually needed. But if you live with someone at high risk - like an elderly parent or newborn - getting tested helps you avoid spreading it. Urgent care centers can test you in 15 minutes.
Can I take ibuprofen with Tamiflu?
Yes. Ibuprofen and acetaminophen are safe to take with antivirals. They help with fever and pain but don’t affect how the antiviral works. Avoid aspirin in children and teens due to Reye’s syndrome risk.
What’s the difference between flu and COVID-19 symptoms?
Both cause fever, cough, fatigue, and body aches. But loss of taste or smell is far more common with COVID-19 - seen in 80% of early cases. Flu rarely causes that. Also, nausea and vomiting are more frequent with flu in adults than with most strains of COVID-19. Testing is the only way to know for sure.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.