When a pharmacist fills a prescription, they’re not just handing out pills-they’re making a clinical decision based on a complex web of data. The difference between a brand-name drug and its generic version might seem simple: one costs less, the other has a familiar name. But behind the scenes, pharmacy systems must accurately identify which is which, and get it right every time. Mistakes can lead to safety risks, billing errors, or even patients losing trust in their care. With generics making up 90% of prescriptions filled in the U.S., getting this right isn’t optional-it’s essential.
Why Generic and Brand Identification Matters
It’s easy to assume that a generic drug is just a cheaper copy. But the FDA doesn’t allow that. A generic must match the brand-name drug in active ingredient, dosage, strength, route of administration, and performance. The only differences allowed are in inactive ingredients-like fillers or dyes-which rarely affect patients but can cause issues in rare cases.
Pharmacy systems need to know whether a drug is a brand, a generic, an authorized generic (the exact same drug sold under a different name), or a branded generic (a generic with a marketing name). Confusing these can lead to:
- Wrong substitutions for narrow therapeutic index (NTI) drugs like warfarin or levothyroxine
- Patients being charged more because the system didn’t recognize a generic
- Pharmacists missing out on cost-saving opportunities
- Insurance denials due to incorrect drug coding
According to U.S. Pharmacist, generic drugs saved the U.S. healthcare system nearly $2 trillion between 2009 and 2019. But that savings only happens if systems correctly identify and promote the right options.
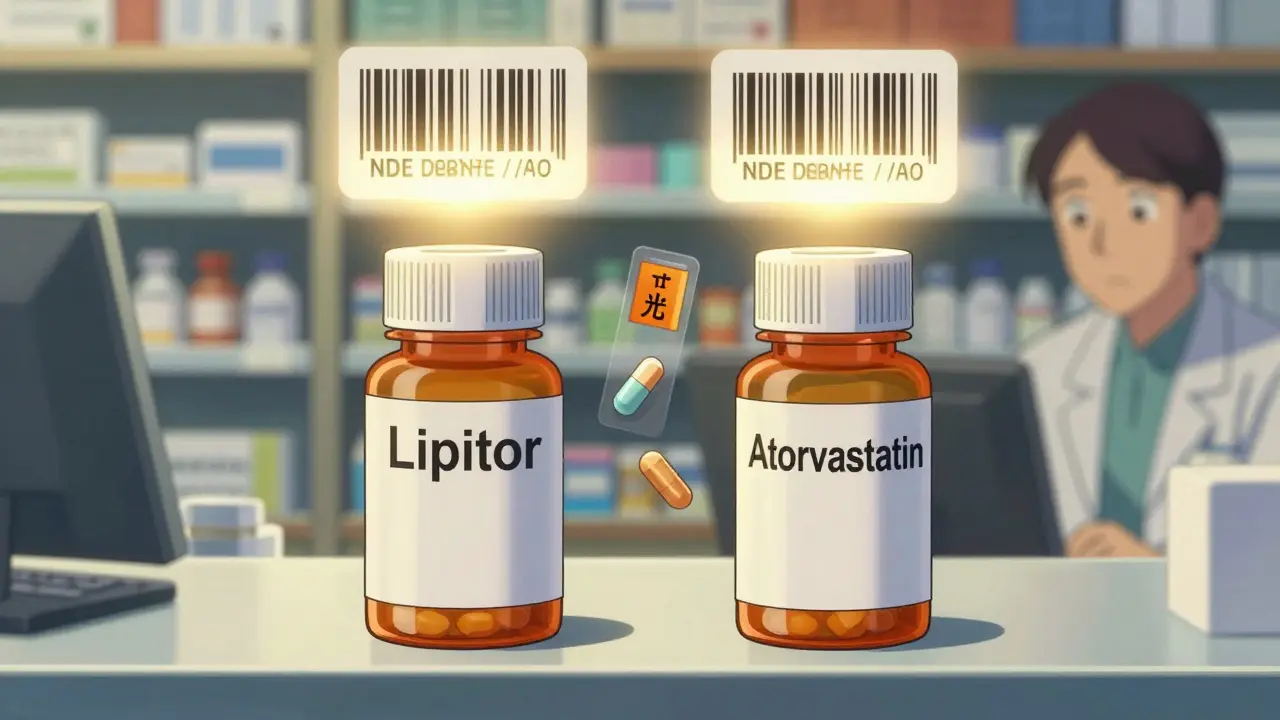
The Role of the National Drug Code (NDC)
Every drug in the U.S. has a unique 10- or 11-digit National Drug Code (NDC). This isn’t just a barcode-it’s the key identifier that links a specific product to its manufacturer, strength, and formulation.
For example:
- Brand-name Lipitor (atorvastatin) might have NDC 50458-0224-01
- A generic version from Teva could be 00603-1975-01
- An authorized generic of Lipitor sold under a different label might be 50458-0224-02
Even though the active ingredient is identical, each NDC is unique. Pharmacy systems must map these correctly. If a system doesn’t recognize that 50458-0224-02 is still Lipitor’s exact formula, it might wrongly flag it as a different drug-or worse, not allow substitution when it should.
The FDA updates its NDC Directory over 3,500 times a month. Systems that don’t sync daily risk using outdated codes, leading to dispensing errors. Pharmacies using outdated databases are more likely to encounter claims denials or patient complaints.
Therapeutic Equivalence (TE) Codes: The Secret Sauce
The FDA’s Orange Book doesn’t just list drugs-it assigns each a Therapeutic Equivalence (TE) code. These two-character codes tell systems whether a generic is interchangeable with the brand.
- AB: Bioequivalent and therapeutically equivalent. Can be substituted freely.
- AN: Bioequivalent but not yet rated (usually new generics).
- BN: Not rated-usually because the brand is complex (like inhalers or topical creams).
- AO: Authorized generic-same as brand, just labeled differently.
Pharmacy systems that ignore TE codes are flying blind. A system that defaults to brand-name drugs because it doesn’t recognize an AB-rated generic is costing patients money and violating best practices. The American Society of Health-System Pharmacists (ASHP) recommends systems default to generic names unless clinically inappropriate.
For example, if a patient’s prescription says “Lisinopril 10 mg,” the system should automatically suggest the generic. But if it shows 17 different lisinopril options without indicating which are AB-rated, pharmacists waste time guessing-and patients get confused.
Authorized Generics and Branded Generics: The Hidden Confusion
Not all generics are created equal. Two tricky categories cause major confusion:
- Authorized generics are made by the brand-name company and sold under a generic label. They’re identical in every way-same factory, same ingredients, same packaging. But because they’re labeled generically, systems often treat them as inferior.
- Branded generics are generics that have marketing names like Errin, Jolivette, or Sprintec. They’re not brand-name drugs, but they don’t look like typical generics either. Many patients think they’re getting the original drug.
A 2022 survey found that 78% of pharmacists struggled to distinguish between branded generics like Sprintec and Tri-Sprintec. The system might show them as separate drugs when they’re nearly identical in formulation. This leads to:
- Patients being told they can’t switch because “it’s not the same”
- Prescribers unknowingly writing for a branded generic when a cheaper AB-rated option exists
- Insurance systems rejecting claims because the name doesn’t match the formulary
Systems that integrate the FDA’s “First Generic Drug Approvals” list-which updates weekly-have a major advantage. They know about new generics before the Orange Book catches up, letting pharmacists offer savings earlier.
Narrow Therapeutic Index (NTI) Drugs: When Substitution Isn’t Safe
Some drugs have a razor-thin margin between effective and toxic doses. These are called narrow therapeutic index (NTI) drugs. Examples include:
- Warfarin (blood thinner)
- Phenytoin (seizure control)
- Levothyroxine (thyroid hormone)
- Cyclosporine (organ transplant)
Even tiny differences in absorption can cause serious harm. While the FDA says AB-rated generics are safe, some patients report changes in how they feel after switching-even when the generic is technically equivalent.
Systems like Epic and Cerner now include specific alerts for NTI drugs. They prevent automatic substitution and require pharmacist review. But not all systems do this. A 2021 ISMP report found 147 adverse events linked to inappropriate generic substitution of warfarin over 18 months, mostly because the pharmacy system didn’t block the switch.
Best practice? If the drug is NTI, the system should:
- Flag it clearly
- Prevent automatic substitution
- Require pharmacist confirmation
- Log why a brand was kept
Kaiser Permanente’s system does this well. Their pharmacy workflow automatically defaults to generics-but for NTI drugs, it pops up a warning: “Patient has previously used brand. Confirm substitution.” This reduces errors without slowing down care.
State Laws and System Compliance
Every state has its own rules about when pharmacists can substitute generics. Forty-nine states allow substitution without prescriber approval if the drug is AB-rated. But the rules vary:
- California: Pharmacists must document why a brand was kept in the patient record.
- Texas: No documentation needed-automatic substitution is allowed.
- New York: Requires the patient to be notified before substitution.
Pharmacy systems must be configured to follow each state’s laws. A national chain can’t use the same settings everywhere. Systems that don’t adapt to state rules risk legal liability and compliance fines.
Centers for Medicare & Medicaid Services (CMS) now require all Part D pharmacy systems to integrate FDA Orange Book TE codes with 99.5% accuracy. That means your system must be updated daily, check every prescription, and flag mismatches.
What Works: Real-World Examples
Some organizations have nailed this. Kaiser Permanente’s system has a 92.7% generic dispensing rate. How? They:
- Default to generics in all order screens
- Use visual comparison tools that show brand vs. generic side by side
- Include patient education pop-ups that explain bioequivalence
- Allow prescribers to override with one click
The result? A 37% drop in brand continuation requests. Patients understand why generics are safe-and choose them.
Humana’s system uses “therapeutic interchange” logic. When a prescriber writes for a brand, the system suggests: “A generic is available and covered. Would you like to switch?” If the prescriber says no, it logs the reason. This increased generic use by 22% without increasing errors.

Common Pitfalls and How to Fix Them
Here are the top mistakes pharmacies make-and how to avoid them:
- Mistake: Relying on drug names alone. Fix: Always check the NDC and TE code. A drug named “Lisinopril” could be brand, generic, or authorized generic.
- Mistake: Ignoring inactive ingredients. Fix: For patients with allergies or sensitivities, cross-check excipients using DailyMed data.
- Mistake: Not training staff on authorized generics. Fix: Run quarterly 30-minute training sessions. Use real examples: “This is the same drug as Lipitor-just labeled differently.”
- Mistake: Using outdated NDC databases. Fix: Sync with the FDA’s API daily. Don’t wait for monthly updates.
- Mistake: Forgetting patient communication. Fix: Always explain substitutions. A simple: “This is the same medicine, just cheaper” cuts complaints by 60%.
According to Consumer Reports, 89% of patients were satisfied with generic substitutions when they understood why. Only 63% were satisfied when they weren’t told anything.
What’s Next: AI and the Future of Drug Identification
The FDA is moving toward real-time API updates for the Orange Book, cutting the 2-3 week lag to near-instant. By 2026, pharmacy systems will pull live data directly from the FDA.
AI tools are already predicting substitution risks. One system published in the Journal of the American Medical Informatics Association uses prescription patterns to flag potential issues with NTI drugs. It’s 87.3% accurate.
Long-term, pharmacogenomics may play a role. If a patient has a genetic marker that affects how they process a drug, the system could auto-flag: “Brand recommended due to CYP2C19 variant.”
The market for pharmacy identification software is growing fast-projected to hit $2.8 billion by 2028. The companies leading this are LexID and Medi-Span, which power over 75% of hospital systems.
But technology alone won’t fix this. It takes trained staff, clear policies, and patient-centered communication. The goal isn’t just to save money-it’s to ensure every patient gets the right drug, every time, with confidence.
Can a generic drug be worse than the brand?
No, if it’s FDA-approved and rated AB. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand. Studies show no difference in effectiveness or safety for the vast majority of patients. A few patients may report feeling different after switching-often due to changes in inactive ingredients or psychological factors-but this doesn’t mean the generic is inferior.
Why do some pharmacies charge more for generics?
This usually happens when the pharmacy’s system doesn’t recognize the generic as covered under the patient’s insurance. It might be due to an outdated NDC, incorrect TE code, or mismatched formulary. Always check the prescription label and insurance status. If the generic is approved and AB-rated, it should cost less. If it doesn’t, ask the pharmacist to verify the NDC and insurance tier.
What’s the difference between an authorized generic and a regular generic?
An authorized generic is made by the original brand-name manufacturer and sold under a generic label. It’s identical in every way-same factory, same ingredients, same packaging. A regular generic is made by a different company but meets FDA bioequivalence standards. Authorized generics often have fewer complaints because patients recognize the formulation, even if the label is different.
Do all pharmacy systems automatically substitute generics?
No. Systems can be configured to default to generics, but they must also respect prescriber instructions and state laws. Some prescribers write “Dispense as Written” (DAW) or “Brand Necessary.” Systems should honor these. Best systems allow substitution unless blocked by law, prescriber, or clinical risk (like NTI drugs).
How can I tell if my pharmacy is using the right generic?
Check the drug label. Look for the manufacturer name and NDC number. Compare it to the brand-name version. If the active ingredient and strength match, it’s correct. Ask your pharmacist: “Is this an AB-rated generic?” If they can’t answer, it’s a red flag. You can also check the FDA’s Orange Book online using the drug name and manufacturer.
Next Steps for Pharmacies
- Review your system’s TE code integration-make sure it pulls from the FDA’s live API.
- Train staff monthly on authorized generics, branded generics, and NTI drug flags.
- Implement patient education: use simple visuals to show how generics are the same.
- Audit your NDC database weekly for outdated codes.
- Ensure your system enforces state substitution laws correctly.
Pharmacy systems are only as good as the data they use and the people who manage them. The goal isn’t just to cut costs-it’s to deliver safe, consistent, and transparent care. When generics are identified correctly, everyone wins: patients, providers, and the system itself.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.