Most people assume that taking an expired pill is harmless-maybe less effective, but not dangerous. That’s a dangerous myth. While the majority of expired medications don’t turn poisonous, a small but critical group can become harmful-or worse, completely useless when you need them most.
Expiration Dates Aren’t Just a Marketing Trick
The date printed on your medicine bottle isn’t arbitrary. It’s the last day the manufacturer guarantees the drug will work as intended and remain safe under proper storage. This requirement came from U.S. law in 1979, and it’s based on real stability testing. But here’s what most people don’t know: the FDA’s Shelf Life Extension Program, which tested over 100 drugs for the Department of Defense, found that 90% of medications still worked perfectly 5 to 15 years past their expiration date-if stored correctly.
That doesn’t mean you should keep every pill forever. The problem isn’t the date itself. It’s the type of medication and how you store it.
The Real Danger: These 5 Medications Can Turn Toxic
Not all drugs degrade the same way. Some just lose strength. Others break down into chemicals that can damage your body. Here are the five that demand your attention:
- Tetracycline antibiotics: In 1963, three people developed kidney damage after taking expired tetracycline. The drug broke down into epitetracycline and anhydro-4-epitetracycline-nephrotoxic compounds that harm the kidneys. While modern packaging reduces this risk, it’s still the only well-documented case of toxicity from expired antibiotics.
- Nitroglycerin: Used for chest pain, this medication turns into unstable nitrogen oxides after expiration. A 2019 Cleveland Clinic study showed it loses half its potency within three months past the date. If you’re having a heart attack and your nitroglycerin doesn’t work, you’re not just out of luck-you’re at risk of death.
- Insulin: After expiration, insulin forms clumps and fibrils. Studies show it loses 20-30% of its effectiveness each year. For diabetics, that means higher blood sugar, more complications, and potentially life-threatening highs or lows.
- Liquid antibiotics: Amoxicillin-clavulanate and other liquid suspensions don’t just weaken-they can grow bacteria. Once opened, they’re only good for 14 days. After that, the preservatives fail. Taking them can cause severe diarrhea, vomiting, or even antibiotic-resistant infections.
- EpiPens: Epinephrine degrades quickly. A 2017 study found that after one year past expiration, EpiPens lose 85% of their potency. If you’re having an allergic reaction and your EpiPen fails, you won’t get a second chance.
What’s Safe? What’s Not
Here’s the good news: most solid medications-like blood pressure pills, antidepressants, antihistamines, and even aspirin-are generally safe to take past their expiration date. The FDA’s data shows they retain 70-90% of their potency for 5-15 years if kept cool and dry.
But even safe drugs have risks. Aspirin breaks down into acetic acid and salicylic acid. After two years past expiration, it’s 50% more likely to irritate your stomach. That’s not toxic, but it’s enough to cause ulcers or bleeding in people with sensitive guts.
On the flip side, eye drops are a silent hazard. Once opened, they’re only good for 28 days. After that, the preservatives die off. Bacteria can grow in the bottle. Using expired eye drops can lead to corneal ulcers and permanent vision loss.

Storage Matters More Than You Think
Where you keep your meds is just as important as when they expire. The FDA says “cool, dry place” means 15-25°C (59-77°F) and 35-45% humidity. That’s not your bathroom. That’s not your bedroom drawer next to the radiator. That’s not your car glove compartment in summer.
Studies show that 78% of people store medications in places that ruin them. Bathrooms average 32°C and 80% humidity-perfect for breaking down pills. A 2022 UCSF study found that insulin stored at room temperature loses 30% more potency than refrigerated insulin. Nitroglycerin tablets in plastic bottles degrade completely in six months. In their original glass containers? They last longer.
Don’t rely on smell or color. A pill that looks fine might be chemically broken down. A liquid that hasn’t changed color could still be contaminated. The only way to know is to check the date-and know what kind of drug you’re dealing with.
What Happens When You Take an Expired Drug?
Most of the time, nothing dramatic. You just don’t get better.
People on Reddit report taking expired allergy meds and still feeling fine. Others say their expired ibuprofen didn’t touch their headache. That’s not a miracle-it’s luck. The drug still had enough active ingredient to help.
But here’s the real cost: treatment failure. A 2023 Consumer Reports survey found 68% of U.S. adults have taken expired meds. Only 0.3% reported toxicity. But 12% said the medicine didn’t work. That’s not a minor inconvenience. That’s someone with asthma using an expired inhaler and ending up in the ER. That’s a parent giving expired antibiotics to a sick child, and the infection spreads because the drug didn’t kill the bacteria.
Dr. Robert S. Hoffman from the New York City Poison Control System put it bluntly: “The real tragedy isn’t poisoned patients from expired drugs-it’s the untreated heart attack because expired nitroglycerin didn’t work when needed most.”
What Should You Do?
Don’t panic. Don’t toss everything. Do this instead:
- Check the date. If it’s expired, ask: What kind of drug is this?
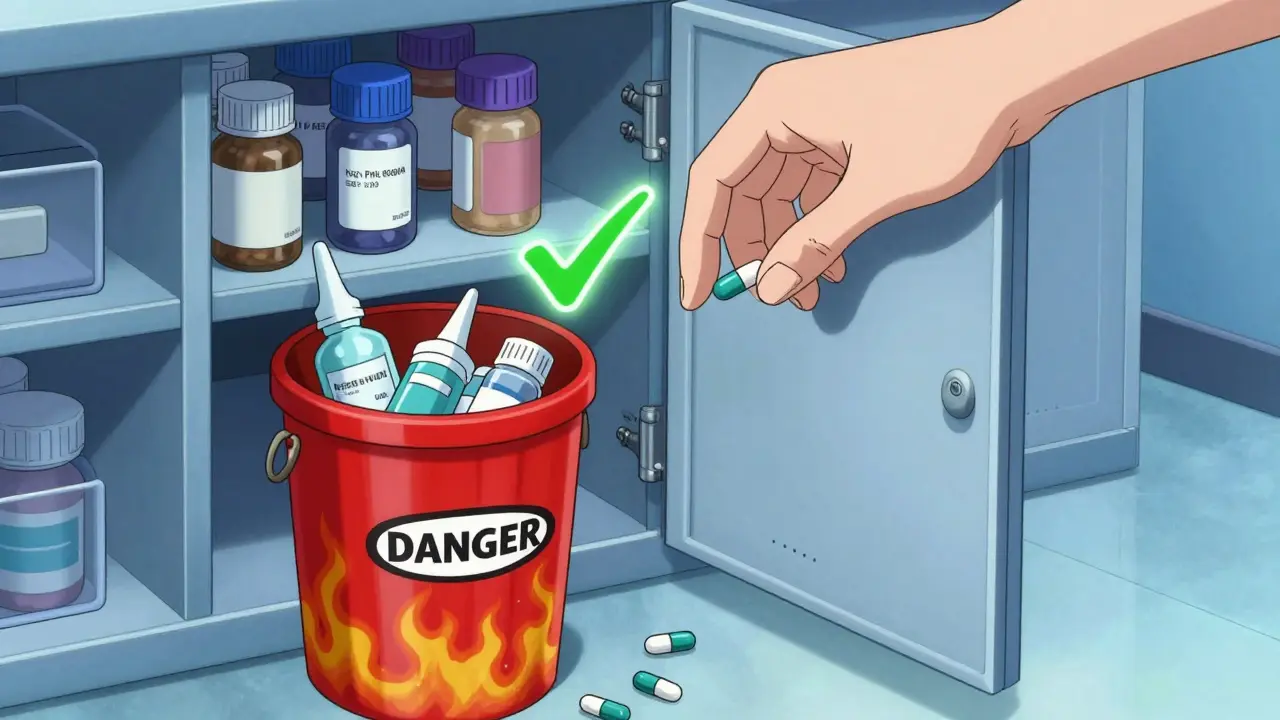
- Throw away nitroglycerin, insulin, EpiPens, liquid antibiotics, and eye drops after expiration. No exceptions.
- Keep solid pills like blood pressure meds, antidepressants, or painkillers if they’ve been stored properly and are only a year or two past expiration. But don’t rely on them for emergencies.
- Store meds right. Use a cool, dry cabinet-not the bathroom, not the kitchen near the stove. Keep them in original containers with the label intact.
- Dispose safely. Don’t flush them. Don’t throw them in the trash. Take them to a pharmacy drop-off or a National Prescription Drug Take-Back Day event. In 2023, over 900,000 pounds of expired meds were collected nationwide.
Why Do Expiration Dates Exist If Most Drugs Last Longer?
The system was built for safety, not efficiency. Manufacturers test drugs for a few years, then add a buffer. It’s conservative by design. But it’s also expensive. The U.S. spends $8.2 billion a year replacing expired drugs that are still good. The Department of Defense saved $1.2 million a year just by extending expiration dates on 10 critical meds.
Some experts say the system is broken. The NIH reviewed 200 studies and found no evidence of toxicity from 98% of medications expired within five years-if stored properly. The American College of Medical Toxicology says only two cases of toxicity from expired drugs have been documented in the last 60 years.
But until the system changes, you have to play it safe. Because when it comes to your health, you don’t want to be the 2%.
What’s Changing?
The future is smarter expiration dates. Companies like Pfizer and Merck are investing hundreds of millions in smart packaging that tracks real-time storage conditions. By 2027, your insulin bottle might say: “Best until June 2026-unless stored above 30°C, use by March 2026.”
The FDA is already running pilot programs to extend expiration dates for 20 critical drugs based on actual stability data. It’s a slow shift, but it’s coming.
Until then, treat expiration dates like traffic lights: red means stop, even if you think you can make it through.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.