Orthostatic Hypotension Calculator
Orthostatic Hypotension Assessment
This calculator determines if your blood pressure drop meets diagnostic criteria for orthostatic hypotension. Enter your supine and standing blood pressure values to see if you meet the criteria (systolic drop ≥20 mm Hg or diastolic drop ≥10 mm Hg within 3 minutes of standing).
When you stand up and feel dizzy or even faint, you might be dealing with idiopathic orthostatic hypotension. It’s more than just a momentary drop in blood pressure - for many it signals an underlying problem with the autonomic nervous system. Recent research shows that this condition often walks hand‑in‑hand with Parkinson’s disease, a neurodegenerative disorder best known for tremors and stiffness. Understanding how the two interact can help patients and clinicians spot warning signs earlier and choose smarter treatments.
Key Takeaways
- Idiopathic orthostatic hypotension is a chronic drop in blood pressure on standing without a clear cause.
- Parkinson’s disease frequently involves autonomic failure, making orthostatic symptoms common.
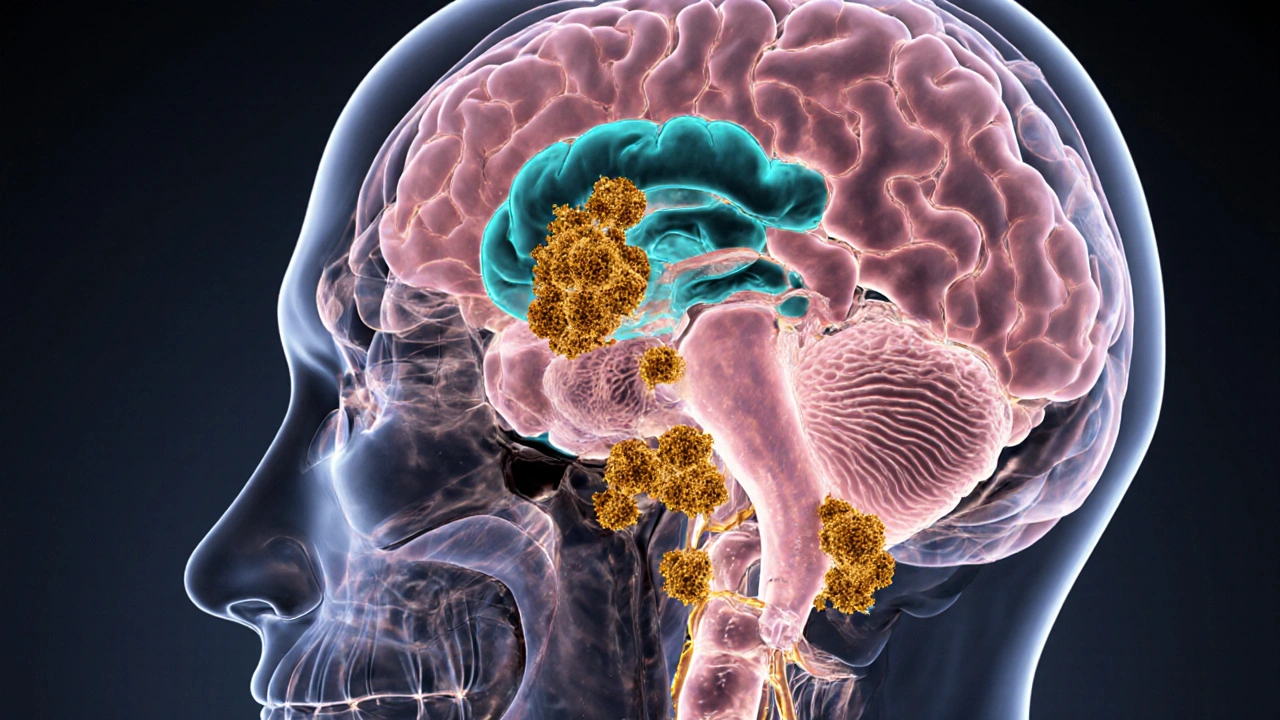
- Alpha‑synuclein deposits in the autonomic nervous system disrupt baroreflex pathways.
- Early identification via tilt‑table testing or continuous blood‑pressure monitoring can improve management.
- Tailored therapy-fluid loading, compression garments, and careful medication adjustment-reduces falls and improves quality of life.
What Is Idiopathic Orthostatic Hypotension?
Idiopathic orthostatic hypotension is defined as a sustained systolic drop of at least 20mmHg or diastolic drop of 10mmHg within three minutes of standing, without an identifiable secondary cause such as dehydration, medication side‑effects, or cardiac disease.
Because the term “idiopathic” means “unknown cause,” clinicians treat it as a primary autonomic failure. The condition reflects an inability of the body’s baroreflex-the rapid feedback loop that normally tightens blood vessels and raises heart rate when you stand-to respond adequately.
Typical symptoms include light‑headedness, blurred vision, fatigue, and in severe cases, syncope (fainting). These episodes often happen after meals, in hot environments, or after prolonged sitting.
Parkinson’s Disease: A Quick Overview
Parkinson's disease is a progressive neurodegenerative disorder characterized by the loss of dopamine‑producing neurons in the substantia nigra, leading to motor symptoms such as bradykinesia, rigidity, tremor, and postural instability.
Beyond the classic motor picture, up to 80% of patients develop non‑motor symptoms, which frequently involve the autonomic nervous system. These include constipation, urinary urgency, sexual dysfunction, and importantly, orthostatic hypotension.
The pathological hallmark is the accumulation of misfolded alpha‑synuclein into Lewy bodies, which spread from the brainstem to peripheral autonomic ganglia.
Why Do the Two Conditions Overlap?
The link hinges on autonomic degeneration. In Parkinson’s disease, alpha‑synuclein aggregates infiltrate the dorsal motor nucleus of the vagus, the intermediolateral cell column of the spinal cord, and peripheral sympathetic ganglia. This damages the neural circuits that regulate blood‑pressure homeostasis.
When the baroreflex is compromised, standing triggers a blunted sympathetic surge, causing the same blood‑pressure dip seen in idiopathic orthostatic hypotension. In other words, the **same pathological process** that produces tremor also sabotages the body’s ability to keep blood flowing to the brain when you rise.
Several epidemiologic studies from 2022‑2024 report that 30‑45% of newly diagnosed Parkinson’s patients already exhibit orthostatic drops meeting the criteria for idiopathic orthostatic hypotension, even before motor symptoms dominate.
Clinical Evidence Connecting IOH and Parkinson’s
Key research findings include:
- Longitudinal cohort studies: A 2023 multi‑center trial followed 412 Parkinson’s patients for five years. Those with baseline orthostatic hypotension progressed to Hoehn‑Yahr stage3 an average of 1.2years earlier than those without.
- Neuropathology: Post‑mortem examinations reveal dense alpha‑synuclein deposits in the cervical sympathetic ganglia of patients who suffered from severe orthostatic hypotension.
- Imaging biomarkers: Da‑Tscan SPECT imaging shows reduced dopamine transporter binding in the basal ganglia correlates with lower baroreflex sensitivity measured by beat‑to‑beat blood‑pressure recordings.
- Genetic overlap: Mutations in the SNCA gene (encoding alpha‑synuclein) are associated with both early‑onset Parkinson’s and familial forms of autonomic failure.
These data collectively argue that idiopathic orthostatic hypotension is not a random comorbidity but rather an early manifestation of the same neurodegenerative cascade that drives Parkinson’s disease.
Diagnosing Orthostatic Hypotension in a Parkinson’s Patient
Because symptoms can be subtle, a systematic approach is vital:
- Baseline vitals: Record supine blood pressure after five minutes of rest, then repeat at 1, 3, and 5 minutes after standing.
- Tilt‑table test: The gold standard. The patient is tilted to 60-70 degrees for up to 10 minutes while continuous non‑invasive blood‑pressure monitoring records the nadir pressure.
- Autonomic function panel: Includes heart‑rate variability, Valsalva maneuver, and quantitative sudomotor axon reflex test (QSART) to gauge sympathetic integrity.
- Medication review: Levodopa, dopamine agonists, and MAO‑B inhibitors can worsen blood‑pressure drops. Adjustments are often needed.
Documenting the exact drop and timing helps distinguish true idiopathic orthostatic hypotension from medication‑induced or volume‑related episodes.

Managing Patients Who Have Both Conditions
Management is a balance between treating Parkinson’s motor symptoms and supporting autonomic function. Strategies fall into three categories: lifestyle, pharmacologic, and device‑based.
Lifestyle Adjustments
- Increase fluid intake to 2-3L per day, focusing on electrolyte‑rich drinks.
- Elevate the head of the bed by 10-15cm to reduce nocturnal blood‑pressure pooling.
- Wear thigh‑high compression stockings (30-40mmHg) during the day.
- Rise slowly: sit for a minute, then stand, allowing the baroreflex a chance to catch up.
- Avoid large meals and hot showers right after waking.
Pharmacologic Options
Drug therapy should be individualized; some agents improve blood pressure but may worsen tremor or hallucinations.
| Drug | Mechanism | Typical Dose | Notes for Parkinson’s |
|---|---|---|---|
| Midodrine | Alpha‑1 agonist - vasoconstriction | 5-10mg PO q8h | May raise supine BP; monitor for supine hypertension. |
| Droxidopa | Prodrug converted to norepinephrine | 100‑600mg PO q6h | Generally well‑tolerated; adjust Parkinson’s meds if dizziness persists. |
| Fludrocortisone | Mineralocorticoid - expands plasma volume | 0.1mg PO daily | Watch for edema and potassium loss. |
| Domperidone (for nausea) | D2 antagonist - improves gastric emptying | 10mg PO q8h | Can modestly raise BP; useful if levodopa causes hypotension. |
Device‑Based Interventions
- Scheduled water bolus: 500ml of cold water can transiently raise BP for ~20minutes.
- Dual‑chamber pacemaker with rate‑responsive programming: In selected patients with severe chronotropic incompetence, pacing improves cardiac output on standing.
- Physical counter‑maneuvers: Leg crossing, squatting, or calf‑muscle tensing can boost venous return.
These tools work best when paired with medication and lifestyle changes.
When to Seek Specialist Care
If a patient experiences:
- Repeated syncope despite basic measures,
- Supine hypertension (systolic >180mmHg),
- Severe falls causing injury,
- Difficulty titrating Parkinson’s meds because of blood‑pressure swings,
refer to a neurologist with a movement‑disorder focus and/or an autonomic specialist. Early referral can prevent complications and refine therapy.
Frequently Asked Questions
Can orthostatic hypotension appear before Parkinson’s motor symptoms?
Yes. Up to one‑third of patients report dizziness or fainting months to years before tremor or stiffness become noticeable. This early autonomic sign can be a red flag for clinicians.
Is it safe to use midodrine together with levodopa?
Midodrine does not directly interact with levodopa, but both can raise blood pressure. Monitoring supine and standing readings is essential to avoid hypertension while still treating the hypotensive episodes.
What non‑drug measure offers the quickest relief during a fainting episode?
Sitting or lying down immediately, raising the legs above heart level, and drinking a glass of cold water can restore cerebral perfusion within seconds.
Do compression stockings interfere with Parkinson’s gait?
Generally no. Modern thigh‑high stockings are thin enough not to restrict movement, and the benefit of reduced blood‑pooling outweighs any minimal impact on stepping.
Is there a genetic test that predicts both conditions?
Testing for SNCA gene multiplications or point mutations can indicate a higher risk for early autonomic failure, but routine screening is not yet standard practice.
Understanding the bridge between idiopathic orthostatic hypotension and Parkinson’s disease turns a vague dizziness complaint into a valuable diagnostic clue. By combining vigilant screening, targeted therapy, and patient‑centered lifestyle tweaks, clinicians can keep blood flowing to the brain-and keep patients moving forward.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.