What Is CKD-Mineral and Bone Disorder?
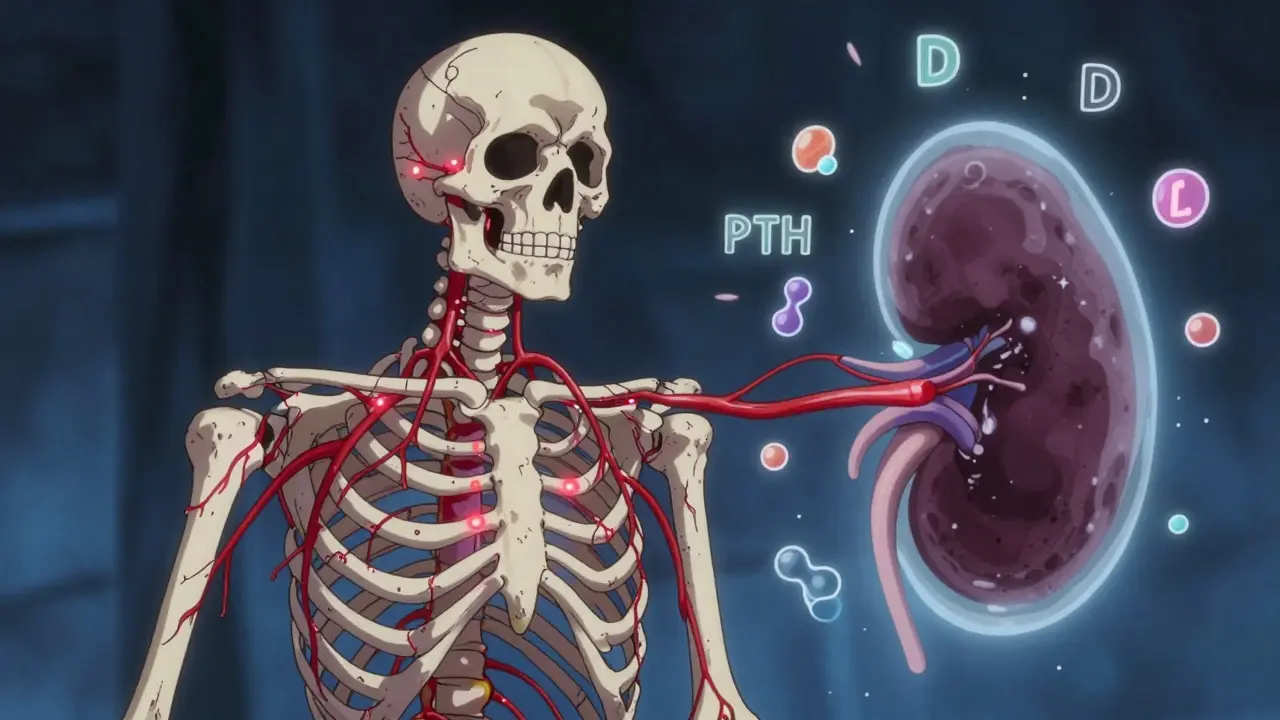
When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your bones and blood chemistry in balance. This isn’t just about weak bones. It’s a whole-system breakdown called CKD-Mineral and Bone Disorder (CKD-MBD). It’s not a single problem. It’s a tangled web of high phosphate, low vitamin D, and runaway parathyroid hormone (PTH), all feeding off each other. And it happens in nearly every person with moderate to advanced kidney disease.
Before 2006, doctors called this condition ‘renal osteodystrophy’-focusing only on bone damage. But we now know the damage goes deeper. Vessels harden. Hearts strain. Fractures become common. This isn’t just a kidney problem. It’s a whole-body crisis tied to three key players: calcium, phosphate, and vitamin D-and the hormone that tries to fix it all: PTH.
The Three-Part Breakdown: Calcium, Phosphate, and Vitamin D
Your kidneys help turn vitamin D into its active form, calcitriol. That’s the version your body uses to pull calcium from food into your blood. When kidney function drops below 60 mL/min (Stage 3 CKD), this process slows. Vitamin D levels crash. Calcium drops. Your body panics.
That’s when the parathyroid glands go into overdrive. They pump out more PTH to pull calcium from your bones. It’s a survival move-but it’s destroying your skeleton. At the same time, your kidneys can’t flush out phosphate anymore. Phosphate builds up. High phosphate + low vitamin D = even more PTH. It’s a loop that gets worse with every passing month.
By Stage 5, when dialysis is needed, over 80% of patients have PTH levels more than three times the normal range. And yet, their bones aren’t getting stronger. Why? Because the bone cells stop responding to PTH. This is called ‘functional hypoparathyroidism’-your body has tons of PTH, but your bones don’t listen. The result? Bone turnover slows. Bones become brittle, even if they look dense on a scan.
Why Vascular Calcification Is the Silent Killer
Here’s the part most people don’t talk about: your arteries are turning to stone. Calcium and phosphate don’t just leach from your bones-they start depositing in your heart, lungs, and blood vessels. This isn’t just plaque. It’s hard, calcified deposits that stiffen arteries and make your heart work harder.
By the time someone reaches dialysis, 75-90% show signs of vascular calcification on a CT scan. Coronary artery calcification scores are 3-5 times higher than in healthy people. And here’s the brutal truth: each 1 mg/dL rise in serum phosphate raises your risk of dying by 18%. That’s not a small risk. It’s the main reason people with advanced kidney disease die before they ever get a transplant.
And it’s not just phosphate. Low vitamin D is just as dangerous. About 80-90% of CKD patients are deficient. That’s not just ‘weak bones’ territory. It’s linked to a 30% higher chance of death. Your immune system, your muscles, your heart-they all need vitamin D to function. When your kidneys can’t activate it, your whole body suffers.
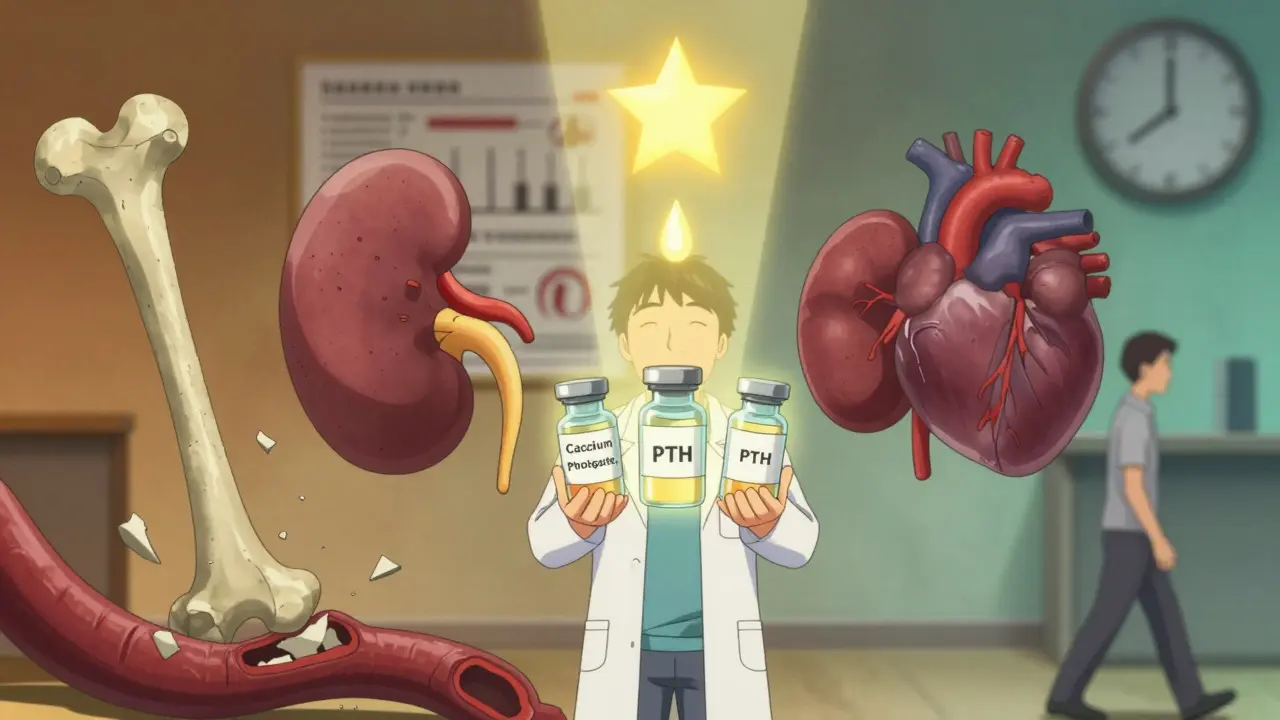
Diagnosing CKD-MBD: What Doctors Actually Check
There’s no single test. Diagnosis means tracking three things over time: calcium, phosphate, and PTH. And vitamin D.
- Calcium: Target is 8.4-10.2 mg/dL. Too low? Your bones break. Too high? Your arteries calcify.
- Phosphate: For early CKD, aim under 4.6 mg/dL. On dialysis? 3.5-5.5 mg/dL. Most patients are over this limit by the time they’re diagnosed.
- PTH: Target is 2-9 times the upper limit of your lab’s normal range. That’s not one number-it varies by assay. But if your PTH is over 800 pg/mL, you’re in high-risk territory.
- 25-hydroxyvitamin D: Keep it above 30 ng/mL. Below 20? You’re severely deficient.
Most doctors don’t do bone biopsies. Too invasive. Instead, they use blood markers like bone-specific alkaline phosphatase (BSAP) and PINP to guess bone turnover. If PTH is low and BSAP is low, you likely have ‘adynamic bone disease’-bone that’s barely remodeling. That’s just as dangerous as high turnover.
Treatment: It’s Not Just Pills
There’s no magic bullet. Treatment has to attack all three sides of the triangle at once.
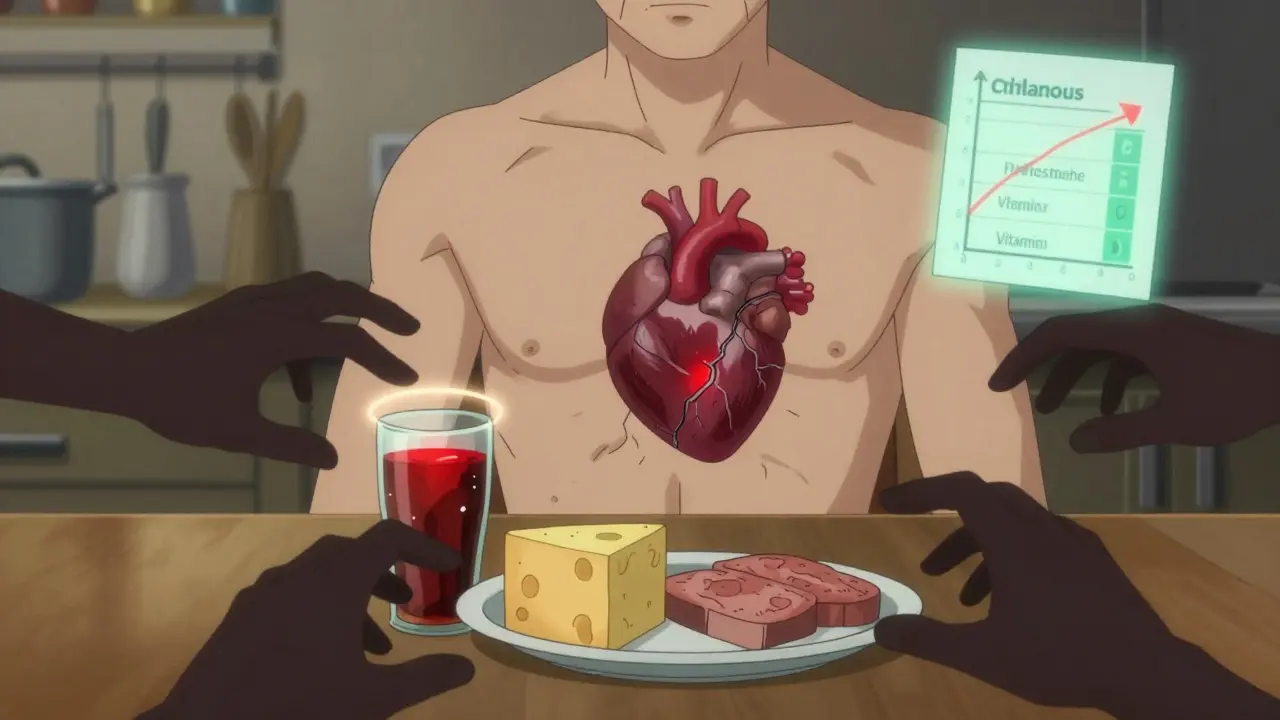
Phosphate control: Diet is first. That means cutting back on processed foods, colas, cheese, and canned meats-all loaded with hidden phosphate. Most people need to stay under 800-1000 mg/day. But diet alone isn’t enough. Phosphate binders are needed. Calcium-based binders (like calcium carbonate) help-but they add more calcium to your blood, which can make calcification worse. So many doctors now use non-calcium binders: sevelamer or lanthanum. They’re pricier, but safer for your heart.
Vitamin D: Don’t jump straight to active forms like calcitriol. That can spike calcium and phosphate. Start with plain vitamin D3 (cholecalciferol)-1000-4000 IU daily. Studies show this lowers death risk by 15% without the side effects. Only use calcitriol or paricalcitol if PTH is sky-high (over 500 pg/mL) and you’re not responding to anything else.
PTH control: If PTH is over 800 pg/mL, calcimimetics like cinacalcet or etelcalcetide can help. These drugs trick the parathyroid gland into thinking calcium is higher than it is-so it stops overproducing PTH. Cinacalcet cuts PTH by 30-50%. Etelcalcetide, a newer injectable, works even better-up to 45% reduction in trials.
The New Frontier: What’s on the Horizon
Research is moving fast. One promising drug targets sclerostin, a protein that blocks bone formation. In CKD, sclerostin levels double. Anti-sclerostin antibodies (like romosozumab) are being tested in early trials-and they’ve boosted bone density by 30-40% in Stage 3-4 patients. That could mean fewer fractures and better mobility.
Another big area: Klotho. This protein helps your kidneys excrete phosphate and protects your heart. In CKD, Klotho drops by 50-70%. Animal studies show giving Klotho reduces calcification by half. Human trials are coming.
And the biggest shift? Starting earlier. CKD-MBD doesn’t wait until dialysis. FGF23-the hormone that signals phosphate overload-starts rising when GFR drops below 60. That’s Stage 3. That’s years before symptoms show. Now, KDIGO recommends checking vitamin D and phosphate every 6-12 months starting at Stage 3. Early action saves lives.
The Bottom Line
CKD-MBD isn’t something you can treat with one pill. It’s not even something you fix. It’s something you manage-daily. Every meal matters. Every blood test counts. Every pill taken-or skipped-changes your future.
High phosphate? It’s not just a lab number. It’s a ticking clock for your heart.
Low vitamin D? It’s not just fatigue. It’s a signal your body can’t protect itself.
High PTH? It’s not just a bone problem. It’s your body screaming for help.
The goal isn’t to get every number perfect. It’s to stop the cycle. To slow the calcification. To keep your bones strong enough to walk, your heart strong enough to pump, and your life long enough to matter.
And that starts with understanding: your kidneys don’t just filter. They balance. When they fail, everything else unravels. But with the right approach, you can hold the pieces together.
Is CKD-MBD the same as osteoporosis?
No. Osteoporosis is bone loss from aging or hormonal changes, usually with normal mineral levels. CKD-MBD is caused by kidney failure and involves high phosphate, low vitamin D, and abnormal PTH. Bone in CKD-MBD can be weak, dense, or both-and it’s often mixed with dangerous calcification in blood vessels, which doesn’t happen in typical osteoporosis.
Can I fix CKD-MBD with supplements alone?
No. While vitamin D supplements help, they’re not enough. Phosphate binders, diet changes, and sometimes medications like calcimimetics are needed. Taking extra calcium without controlling phosphate can actually make vascular calcification worse. Always work with a nephrologist or renal dietitian.
Why do I need to avoid colas and processed foods?
Colas and processed foods contain added phosphate as a preservative or flavor enhancer. This phosphate is almost 100% absorbed by your body-even more than phosphate from meat or dairy. Your kidneys can’t clear it, so it builds up fast. One can of cola can contain 40-50 mg of added phosphate. That’s 5-6% of your daily limit.
How often should I get my calcium, phosphate, and PTH checked?
If you have Stage 3 or 4 CKD, check every 6-12 months. Once you’re on dialysis (Stage 5D), check monthly. Vitamin D should be tested at least once a year, or more if you’re deficient. Frequent monitoring catches problems before they cause damage.
Does dialysis fix CKD-MBD?
Not really. Dialysis removes some phosphate, but not enough to keep up with modern diets. It doesn’t fix vitamin D activation or PTH overproduction. Many dialysis patients still have high phosphate, low vitamin D, and high PTH. That’s why diet, binders, and medications are still needed-even on dialysis.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.