INR Target Range Calculator
INR measures your blood's clotting ability. Your target range depends on why you're on blood thinners.
Why it matters:
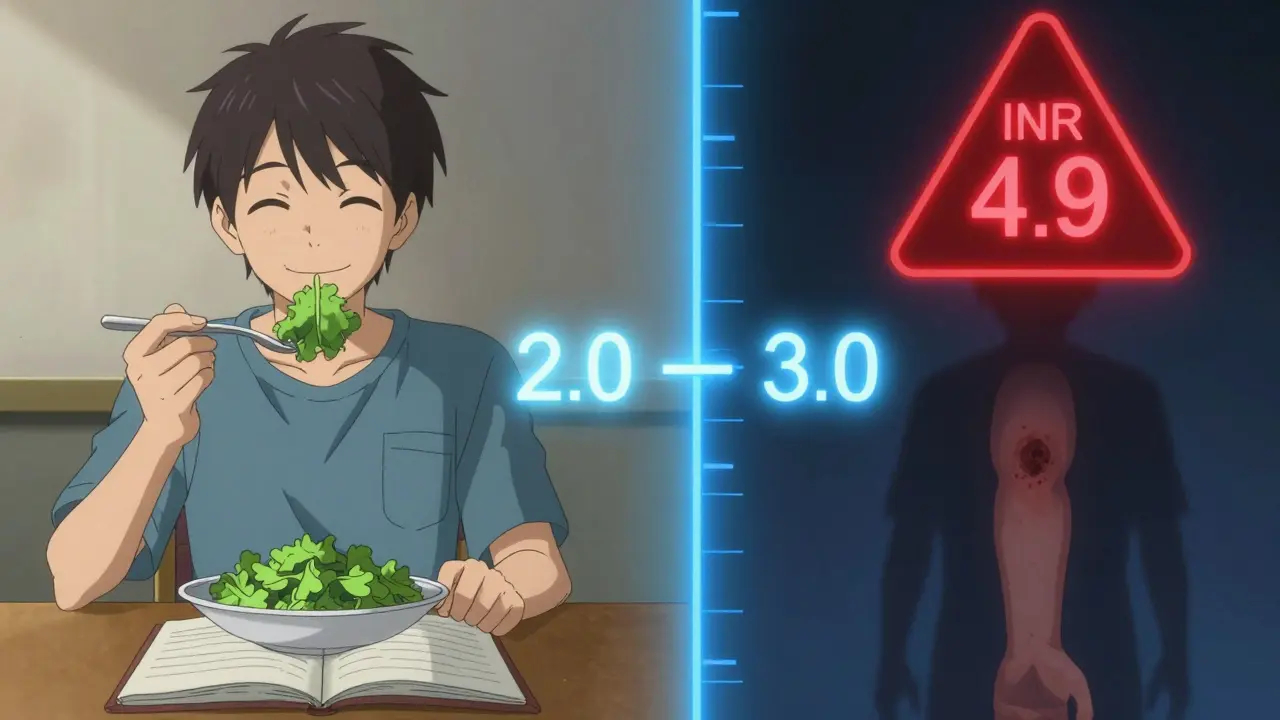
INR below 1.5 = high clot risk (stroke). INR above 4.9 = high bleeding risk.
When you're on a blood thinner like warfarin, your life doesn't just revolve around taking a pill each day. It revolves around a number: your INR. This isn't just a lab result. It's a critical measure that tells you whether you're protected from dangerous clots or at risk of serious bleeding. Get it wrong, and the consequences can be life-threatening. Get it right, and you can live normally-go hiking, travel, play with your grandkids-without constant fear.
What Exactly Is INR?
INR stands for International Normalized Ratio. It's a standardized way to measure how long it takes your blood to clot. Think of it like a traffic light for your blood’s clotting ability. Green means you're in the safe zone. Yellow means you need to pay attention. Red means stop and call your doctor.
Before INR was invented in 1983, every lab reported clotting times differently. One hospital’s “normal” was another’s “dangerously high.” That led to dangerous mistakes. The WHO created INR to fix that. Now, no matter where you test-whether it’s a hospital in Perth, a clinic in Sydney, or your own kitchen table-the same INR number means the same thing. A result of 2.5 is 2.5 everywhere.
The calculation sounds technical: INR = (Patient PT ÷ Mean Normal PT)^ISI. But you don’t need to remember the formula. What matters is this: your PT (prothrombin time) is measured in seconds. Normal is around 11-13.5 seconds. Your INR turns that into a universal number that doctors can trust.
Your Target Range: It’s Not One-Size-Fits-All
Most people on warfarin are told to aim for an INR between 2.0 and 3.0. But that’s not universal. Your target depends entirely on why you’re on blood thinners in the first place.
- If you have atrial fibrillation or a deep vein thrombosis (DVT), your target is usually 2.0-3.0.
- If you have a mechanical heart valve-especially in the mitral position-your target jumps to 2.5-3.5. That’s because these valves are more likely to cause clots.
- If you have a mechanical aortic valve, you’re still usually in the 2.0-3.0 range, though some cases may need higher.
Why the difference? It’s all about risk. Atrial fibrillation increases stroke risk by 5 times. Mechanical valves? Up to 10 times higher. The higher the risk, the more you need to thin the blood. But there’s a trade-off: the higher the INR, the greater the chance of bleeding. That’s why precision matters.
What Happens When Your INR Is Too High or Too Low?
INR below 1.5? That’s too low. Your blood is clotting too fast. You’re at risk of a stroke, heart attack, or pulmonary embolism. One study showed that patients with INR under 1.5 had 3 times higher risk of clot-related hospitalization.
INR above 4.9? That’s dangerous. At this level, even a small bump can cause internal bleeding. Every 0.5-point increase above 3.0 raises your risk of major bleeding by 27%. An INR over 5.0 is an emergency. You may need to skip your next warfarin dose and contact your doctor immediately. Some patients need vitamin K or even a blood transfusion.
And here’s something most people don’t realize: your INR can swing wildly from one test to the next. A drop from 3.2 to 2.6 might seem small-but if you’re on the edge of your target range, that’s enough to make you vulnerable to clots. That’s why consistency matters more than perfection.
Home Testing: Is It Worth It?
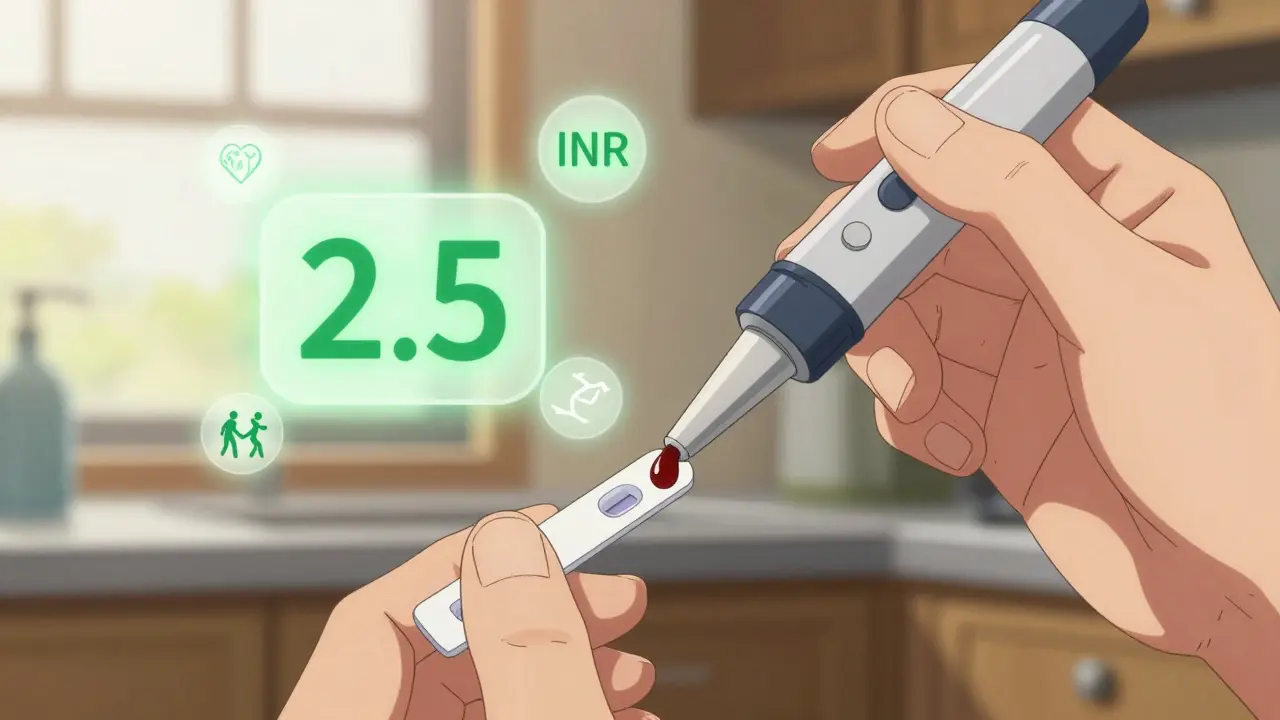
For years, you had to drive to a clinic, wait hours, and get results days later. Now, devices like the Abbott Acelis or Roche CoaguChek let you test at home with a tiny drop of blood from your finger. You get results in under a minute.
The data is clear: people who test at home spend 72% of their time in the target range. Clinic-based patients? Only 58%. That difference cuts stroke risk by 34% and major bleeding by 21%.
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering how to use the device, home testing can backfire. The FDA found that 12% of home devices give inaccurate readings above INR 4.0. And if you misread the result, you might adjust your dose wrong-leading to disaster.
Cost is another factor. The device costs around $299. Each test strip is $5.99. Medicare covers 100% for eligible patients. Private insurance usually covers 80%, leaving you with 20% coinsurance. That’s $100-$300 a year for most people. For many, it’s worth it. One Reddit user said home testing saved them $187 per clinic visit-and cut their anxiety in half.
Warfarin vs. Newer Blood Thinners
Twenty years ago, warfarin was the only option. Today, there are DOACs-direct oral anticoagulants-like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa). These don’t require INR monitoring. That’s why 70% of new prescriptions are for DOACs now.
But here’s the catch: DOACs aren’t right for everyone. If you have a mechanical heart valve, you can’t use them. If you have severe kidney disease, most DOACs are off the table. And if you’re on a tight budget? Warfarin costs $4 a month. DOACs? $550-$650.
DOACs have wider therapeutic windows. You don’t need to hit a narrow target. Warfarin? You’re balancing on a tightrope. A 0.5-point swing can mean the difference between safety and crisis. That’s why INR monitoring isn’t just a chore-it’s your lifeline.
How to Stay in Range
Keeping your INR steady isn’t about luck. It’s about routine.
- Test at the same time of day. Ideally between 8 a.m. and 12 p.m.
- Fasting for 4-6 hours before testing helps. Food, especially leafy greens, changes vitamin K levels, which directly affects warfarin.
- Keep your diet consistent. One week you eat salads every day? Next week, nothing green? Your INR will bounce.
- Tell your doctor about every new medication-even over-the-counter painkillers. Ibuprofen and even some herbal supplements can interfere.
- Use a logbook or app. Track your INR, dose, diet, and symptoms. Patterns reveal problems before they become emergencies.
One patient in Perth noticed his INR kept rising every winter. He realized it was because he stopped walking due to cold weather. Less movement = slower blood flow = higher clotting risk. His doctor adjusted his dose. Simple fix. Big difference.
What to Do If Your INR Is Off
Don’t panic. But don’t ignore it.
- INR below 1.5: Contact your doctor immediately. You may need a higher dose or a temporary boost.
- INR between 3.1-4.9: Skip your next warfarin dose. Retest in 2-3 days. Avoid NSAIDs (like ibuprofen) and alcohol.
- INR above 5.0: Skip your dose. Call your doctor today. You may need vitamin K or urgent care.
Never adjust your dose based on a single test. One outlier doesn’t mean your treatment is broken. Look at trends. Three high readings? Time to talk. One high reading? Wait and retest.
The Bigger Picture: Why This Matters
INR monitoring isn’t just about numbers. It’s about control. It’s about knowing you’re not just surviving-you’re living. Patients who stay in range for over 70% of the time cut their stroke risk by 60%. Hospitals with TTR (time in therapeutic range) above 65% have 42% fewer emergency visits.
And yet, 38% of patients are tested too often. Stable patients don’t need weekly checks. Monthly is enough. Over-testing doesn’t make you safer-it just adds stress, cost, and time.
The future is changing. Smartphone-connected devices now auto-send results to your doctor. AI tools predict your next dose with 83% accuracy. But none of that replaces your role. You’re the one who notices the bruise you didn’t get from bumping into anything. You’re the one who remembers to eat the same amount of greens. You’re the one who calls when something feels off.
This isn’t a burden. It’s your power.
What is a normal INR if I’m not on blood thinners?
If you’re not taking any anticoagulant medication, your normal INR is 1.0. This means your blood clots at the standard rate. Any number above 1.0 indicates your blood is taking longer to clot, which is intentional when you’re on warfarin. A reading of 1.0 is what labs use as the baseline to calculate your therapeutic INR range.
Can I eat leafy greens while on warfarin?
Yes, but keep your intake consistent. Leafy greens like spinach, kale, and broccoli are high in vitamin K, which counteracts warfarin. Eating a lot one week and almost none the next will cause your INR to swing. You don’t need to avoid them-just eat about the same amount every day. A half-cup of cooked greens daily is a good rule of thumb for most people.
How often should I test my INR?
It depends on your stability. When you first start warfarin or after a dose change, you may need testing twice a week. Once you’re stable-meaning your INR stays within range for 2-3 months-monthly testing is usually enough. Some patients on home monitors test weekly, but only if advised by their doctor. Unnecessary weekly testing increases anxiety without improving safety.
Is home INR testing covered by insurance?
In Australia, Medicare does not currently cover home INR testing devices or strips. However, some private health insurers may offer partial rebates under extras cover. In the U.S., Medicare Part B covers 100% of home INR testing for eligible patients, and most private insurers cover at least 80%. Always check with your provider, and ask your doctor to submit a letter of medical necessity if your claim is denied.
Why can’t I use DOACs if I have a mechanical heart valve?
DOACs (like Eliquis or Xarelto) haven’t been proven safe or effective for people with mechanical heart valves. In clinical trials, patients on DOACs with mechanical valves had significantly higher rates of blood clots and valve-related complications compared to those on warfarin. Warfarin remains the only anticoagulant with decades of proven safety for this specific group. Switching without medical guidance can be life-threatening.
What should I do if I miss a warfarin dose?
If you miss a dose, don’t double up the next day. If you remember within 8 hours of your usual time, take it then. If it’s later than that, skip the missed dose and take your next scheduled dose at the regular time. Keep a log of missed doses and mention them at your next INR test. Missing one dose rarely causes a major change-but repeated misses can push your INR out of range.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.