When you hear the word obesity, most people think of weight alone. But the real danger isn’t just the number on the scale-it’s what that extra weight does to your body over time. For millions of people, obesity isn’t just a condition. It’s the starting point for a chain reaction that leads to diabetes, heart disease, and sleep apnea. These three problems don’t just happen alongside obesity-they feed off each other, making everything worse. And the worst part? Many people don’t even know they have all three until something serious happens.
The Hidden Triad: How Obesity Triggers Diabetes, Heart Disease, and Sleep Apnea
Obesity is defined as a body mass index (BMI) of 30 or higher. But it’s not just about being heavy. It’s about fat, especially around the belly, changing how your body works. Fat tissue isn’t harmless padding-it’s active. It releases chemicals that cause inflammation, mess with your hormones, and clog your blood vessels. That’s why obesity is the root of the so-called “comorbidity triad”: type 2 diabetes, cardiovascular disease, and obstructive sleep apnea. Let’s start with sleep apnea. When you carry extra weight, especially around your neck and throat, your airway gets squeezed. Studies show that for every 1-point increase in BMI, your risk of sleep apnea goes up by 14%. In severe obesity, the airway can shrink by 20-30%. That means during sleep, your throat collapses repeatedly-sometimes hundreds of times a night. Your brain wakes you up just enough to breathe, but you never get real rest. This isn’t just about snoring. It’s about your body being starved of oxygen, over and over. That oxygen deprivation doesn’t stay in your throat. It floods your bloodstream, stressing your heart and pancreas. Your blood pressure spikes at night-sometimes by 25 mmHg. Your body starts resisting insulin, the hormone that controls blood sugar. That’s how obesity leads to type 2 diabetes. In fact, obese individuals have 30-50% higher levels of inflammatory markers like C-reactive protein, which directly interfere with insulin function. And it’s not just obesity causing diabetes. The reverse is true too: diabetes can worsen sleep apnea by damaging the nerves that control your airway muscles. Then there’s the heart. Obesity makes your heart work harder. Your left ventricle thickens by 15-20%. Sleep apnea adds more pressure, with nighttime surges that strain your arteries. Diabetes speeds up plaque buildup. Together, they create a perfect storm. People with all three conditions have a 3.2 times higher risk of heart attack than someone with obesity alone. And if you have sleep apnea on top of diabetes and obesity? Your risk of heart failure jumps to 3.7 times higher.Why Doctors Miss This Connection (And How to Fix It)
Here’s the frustrating truth: most doctors treat each condition separately. You see your endocrinologist for diabetes. Your cardiologist for high blood pressure. Your primary care doctor for weight. But very few ask about your sleep. A 2022 study found that only 17.8% of obese people with diabetes get screened for sleep apnea-even though 60-80% of them have it. Why? Because the symptoms are easy to ignore. You’re tired? “You’re overweight, of course you’re tired.” You wake up gasping? “Must’ve been a bad night.” You snore loudly? “Everyone snores.” But the reality is, if you’re obese and have diabetes, you’re almost certainly undiagnosed with sleep apnea. And that’s dangerous. The good news? There’s a simple tool doctors can use: the STOP-Bang questionnaire. It asks about snoring, tiredness, observed breathing pauses, high blood pressure, BMI, age, neck size, and gender. A score of 3 or higher means you need a sleep study. No fancy machines. Just a few questions. Yet, most practices don’t use it. If you’re obese and have diabetes, don’t wait for your doctor to bring it up. Ask: “Could I have sleep apnea?” If you’re constantly tired, wake up with headaches, or your partner says you stop breathing at night, you owe it to yourself to get checked.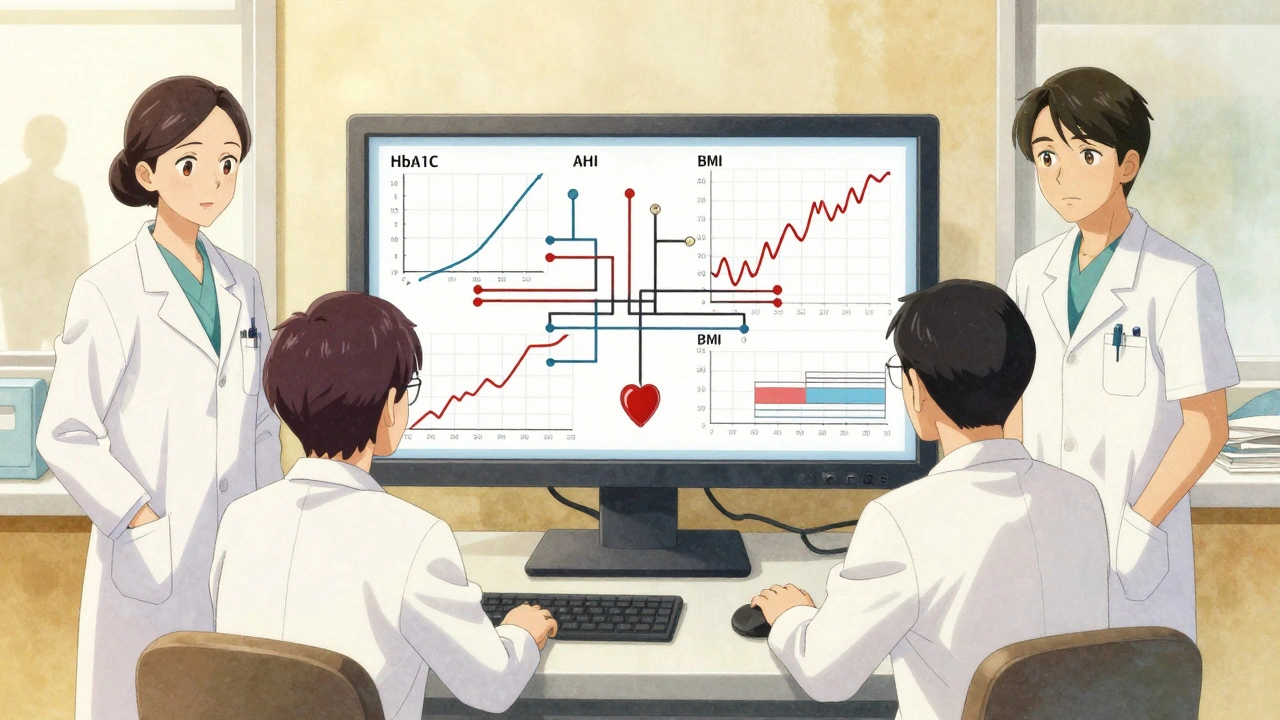
Breaking the Cycle: What Actually Works
The good news? This triad isn’t a death sentence. It’s a cycle-and cycles can be broken. Weight loss is the most powerful tool. Losing just 10-15% of your body weight can cut sleep apnea severity in half. In one study, obese patients with diabetes who lost that much weight saw their AHI (a measure of breathing interruptions) drop by an average of 25.7 events per hour. That’s not just a number-it means you’ll sleep better, feel more alert, and your blood sugar will stabilize. But weight loss is hard. And that’s where treatment for sleep apnea helps. Continuous positive airway pressure (CPAP) isn’t just for snoring. It’s life-saving. People who use CPAP for at least 4 hours a night reduce their risk of heart attack and stroke by 28%. One study showed that after six months of consistent CPAP use, people with diabetes and sleep apnea dropped their HbA1c (a key diabetes marker) by 0.8%. That’s like adding a new medication-without the side effects. And now, there’s even better news. New diabetes drugs like semaglutide (Wegovy, Ozempic) don’t just help you lose weight-they directly improve sleep apnea. In the 2024 LEADER-OSA trial, patients lost nearly 15% of their body weight on average, and their sleep apnea improved even beyond what the weight loss alone explained. Why? Because the drugs reduce fat in the upper airway. That’s groundbreaking. For those who can’t tolerate CPAP, there’s a new option: a hypoglossal nerve stimulator. It’s a small device implanted in your chest that gently stimulates the tongue muscle during sleep to keep your airway open. Clinical trials show 79% of users get more than half of their breathing events reduced.What Doesn’t Work (And Why People Give Up)
Let’s be honest: many people try CPAP and quit. A 2023 study found only 45% stick with it after a year. Why? Masks are uncomfortable. The air pressure feels strange. Some feel claustrophobic. Others just can’t get used to it. But here’s the thing: CPAP doesn’t have to be perfect. Even using it 3 hours a night helps. And there are dozens of mask styles-nasal pillows, full-face, hybrid. If one doesn’t work, try another. Your sleep specialist can help you find the right fit. Weight loss programs that promise quick results? They rarely last. The SLEEP-AHEAD trial showed that the most effective approach was 175 minutes of exercise a week plus a calorie-controlled diet. That’s not magic. That’s consistency. Walking 30 minutes five days a week, cutting out sugary drinks, eating more vegetables-small, daily choices add up. And here’s the kicker: many people lose weight, feel better, and stop doing the things that helped them. That’s when the triad creeps back. This isn’t a fix. It’s a lifestyle.
The Bigger Picture: Why This Matters Beyond Your Health
This isn’t just about you. It’s about the system. Obese patients with all three conditions spend $12,300 more per year on healthcare than those with obesity alone. Most of that is from heart attacks, strokes, hospital stays, and emergency visits. Hospitals that treat these conditions together-like Kaiser Permanente-have cut hospitalizations by 22% and ER visits by 18% in just one year. That’s not just saving money. It’s saving lives. The future is integrated care. A team of doctors: an endocrinologist for diabetes, a sleep specialist for apnea, a cardiologist for heart health, and a dietitian for weight. All talking to each other. All tracking your AHI, HbA1c, blood pressure, and weight in one place. That’s the gold standard. And it’s coming. The American Heart Association now says sleep apnea should be treated like high cholesterol or high blood pressure-because it is. Routine screening for sleep apnea in obese patients with heart disease or diabetes isn’t optional anymore. It’s essential.What You Can Do Today
If you’re overweight and have diabetes-or even if you just suspect you might-here’s your action plan:- Ask your doctor for a STOP-Bang screening for sleep apnea. If your score is 3 or higher, push for a sleep study.
- If you’re diagnosed with sleep apnea, don’t refuse CPAP because it feels weird. Try different masks. Give it 2 weeks. It gets easier.
- Start moving. Walk 30 minutes a day. Five days a week. That’s 150 minutes. It’s not enough to lose 50 pounds overnight, but it’s enough to start reversing damage.
- Cut out sugary drinks. One soda a day adds 15 pounds a year. Replace it with water, tea, or sparkling water.
- Track your progress: weight, HbA1c, and how rested you feel. Small wins matter.
Is sleep apnea only a problem for people who are very overweight?
No. While obesity is the biggest risk factor-accounting for about 70% of cases-25-30% of people with sleep apnea are not overweight. Factors like jaw structure, neck size, age, and genetics also play a role. But if you’re obese, your chances of having sleep apnea are much higher. That’s why screening is critical for anyone with a BMI over 30, especially if they also have diabetes or high blood pressure.
Can losing weight cure sleep apnea and diabetes?
Losing 10-15% of your body weight can dramatically improve both conditions. In many cases, sleep apnea goes into remission, and type 2 diabetes can be reversed to the point where medications are no longer needed. A 2022 study found that 78% of obese patients with sleep apnea saw their condition resolve after bariatric surgery. Even without surgery, consistent weight loss through diet and exercise can cut sleep apnea events in half and lower HbA1c by 1% or more. It’s not a guaranteed cure, but it’s the most effective treatment available.
Why do I feel more tired even after using CPAP?
It can take time for your body to recover from years of poor sleep. Even with CPAP, it may take 4-8 weeks to feel fully rested. Also, if your CPAP pressure is set too low or your mask leaks, you’re still not getting enough treatment. Make sure your device is properly calibrated and your mask fits well. If you’re still tired after a month of consistent use, ask your sleep specialist to check your AHI numbers. You might need a pressure adjustment or a different type of device.
Are there alternatives to CPAP for sleep apnea?
Yes. If you can’t tolerate CPAP, there are other options. Oral appliances that reposition your jaw can help with mild to moderate sleep apnea. For more severe cases, a hypoglossal nerve stimulator (like Inspire) is an implanted device that keeps your airway open during sleep. It’s been shown to reduce breathing events by over 50% in 79% of users. Weight loss is still the most effective long-term solution, but these devices offer real relief for those who can’t use CPAP.
Can diabetes medications help with sleep apnea?
Yes, and this is a recent breakthrough. GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) don’t just help with weight loss-they reduce fat deposits around the upper airway, which directly improves sleep apnea. In the 2024 LEADER-OSA trial, patients on semaglutide saw their sleep apnea improve significantly, even after accounting for weight loss. This means these drugs offer a dual benefit: better blood sugar control and better breathing at night. Talk to your doctor if you’re on diabetes medication and still struggling with sleep.
How do I know if my sleep apnea is getting worse?
Watch for these signs: louder or more frequent snoring, waking up gasping or choking, morning headaches, worsening daytime fatigue, or difficulty concentrating. If you’re using CPAP, your device may track your AHI-check the numbers. If your AHI has increased over time, it could mean your weight has gone up, your mask is leaking, or your condition is progressing. Don’t ignore these signals. Schedule a follow-up sleep study.
Is it safe to use a smartwatch to detect sleep apnea?
Some smartwatches can detect patterns that suggest sleep apnea-like drops in blood oxygen or irregular breathing. But they’re not diagnostic tools. A 2024 study showed smartphone and wearable tracking could predict sleep apnea with 85% accuracy in obese people with diabetes, but they can’t replace a formal sleep study. Use them as a warning sign, not a diagnosis. If your watch shows possible apnea events, talk to your doctor and get a proper test.
Can children develop this comorbidity triad too?
Yes. Childhood obesity is rising, and so is pediatric sleep apnea. Obese children are at higher risk for early insulin resistance and high blood pressure. Untreated sleep apnea in kids can lead to behavioral problems, poor school performance, and early heart strain. If your child is overweight, snores loudly, or sleeps with their mouth open, talk to their pediatrician about a sleep evaluation. Early intervention can prevent lifelong complications.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.