OIC Symptom Tracker & Treatment Guide
OIC Symptom Assessment
This tool helps you track your opioid-induced constipation symptoms and calculate your Bowel Function Index (BFI) score. A score above 30 indicates clinically significant constipation requiring treatment.
Your Results
30-49: Moderate constipation
50+: Severe constipation
When you start taking opioids for chronic pain, you’re told about drowsiness, nausea, and the risk of dependence. But few warn you about the one side effect that can ruin your daily life: opioid-induced constipation. It’s not just a minor inconvenience. For 40 to 60% of people on long-term opioids, it’s a constant, painful reality that doesn’t go away-even after months or years. And unlike other side effects that fade, OIC sticks around because it’s built into how opioids work in your body.
Why Opioids Slow Down Your Gut
Opioids don’t just block pain signals in your brain-they also latch onto receptors in your gut. These receptors, called μ-opioid receptors, are everywhere in your digestive tract. When opioids bind to them, they slow down the natural muscle contractions that move food and waste through your intestines. Your stomach empties slower. Your colon absorbs more water from stool. And your anal sphincter tightens up, making it harder to push anything out.
This isn’t normal constipation. It’s not caused by eating too little fiber or drinking too little water. It’s a direct, chemical effect of the medication itself. That’s why drinking more water or eating prunes often doesn’t help. Your body isn’t just being lazy-it’s being chemically shut down.
When It Starts-and Why Waiting Is a Mistake
Some people notice constipation within days of starting an opioid. Others don’t realize it’s happening until they’ve been straining for weeks. Either way, the damage builds up. Left untreated, OIC can lead to bloating, nausea, vomiting, and even fecal impaction-a dangerous blockage that requires hospitalization.
Here’s the hard truth: if you wait until you’re constipated to start treatment, you’re already behind. Experts agree: you should start a laxative on the same day you start your opioid. A study from Johns Hopkins found that proactive use prevents 60-70% of severe cases. Yet, in most primary care settings, fewer than one in three patients get this advice.
First-Line Treatments: What Actually Works
Most doctors will start you on over-the-counter laxatives. But not all of them are created equal for OIC.
- Polyethylene glycol (PEG) is the top-recommended osmotic laxative. It draws water into the colon without irritating the lining. It’s gentle, effective, and safe for long-term use.
- Stimulant laxatives like senna or bisacodyl help by triggering contractions in the colon. They work faster than PEG but shouldn’t be used daily for more than a few weeks without supervision.
- Stool softeners like docusate? They’re often prescribed, but studies show they do little for OIC. Don’t waste your time.
Many patients think they’re doing the right thing by taking a daily stool softener and calling it good. But if you’re still straining, it’s not working. The key is matching the right tool to the problem-and OIC needs more than just softening.
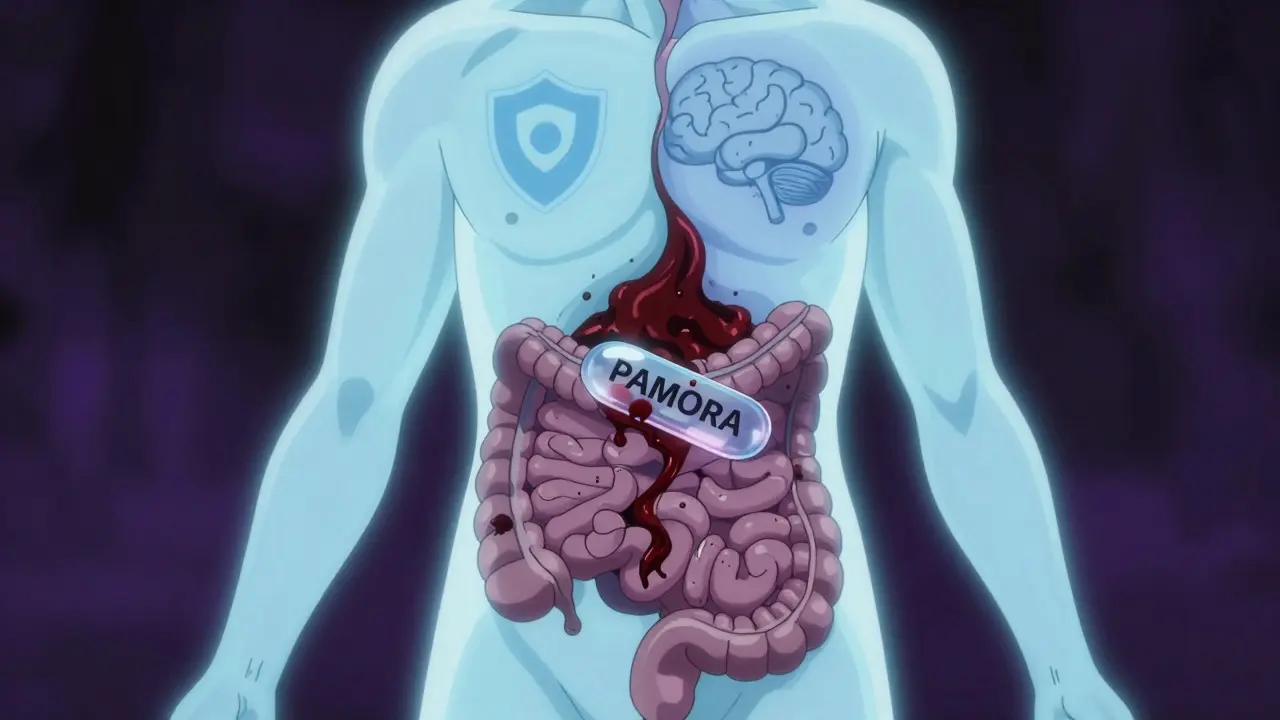
When OTC Isn’t Enough: The Role of PAMORAs
If laxatives aren’t cutting it-and 68% of patients say they aren’t-it’s time to talk about PAMORAs. That’s short for peripherally acting μ-opioid receptor antagonists. These drugs block opioids from acting on your gut, but not your brain. That means your pain relief stays intact, while your bowels get back to normal.
Here are the three main ones:
- Methylnaltrexone (Relistor®): Given as an injection, it works in as little as 30 minutes. Often used in palliative care. A new once-weekly version came out in 2023, making it easier to manage.
- Naldemedine (Movantik®): A daily pill. Approved for cancer patients in 2024 by ASCO guidelines because it also helps reduce opioid-induced nausea. Many users report improved quality of life and fewer bathroom emergencies.
- Lubiprostone (Amitiza®): Works by opening chloride channels in the gut to increase fluid secretion. FDA-approved for women, but studies show it works just as well for men. Side effects? Nausea in 1 out of 3 users.
These aren’t magic bullets. Some people get abdominal cramping or diarrhea. But for those who’ve tried everything else, they’re life-changing.
The Hidden Risks You Need to Know
PAMORAs are powerful-but not safe for everyone. They’re strictly off-limits if you have a bowel obstruction, recent abdominal surgery, or inflammatory bowel disease. There have been real cases of life-threatening bowel perforation linked to these drugs, especially in patients with weakened intestinal walls.
One patient on Reddit shared: “I started Relistor after three months of no bowel movements. It worked instantly-but two days later, I was in the ER with severe pain. Turns out, I had a hidden tear from years of straining.”
That’s why these medications require careful screening. Your doctor should check for signs of chronic obstruction before prescribing them. If you’ve been constipated for over six months, get an imaging test before starting a PAMORA.
Cost, Access, and the Real Barrier to Care
Even when PAMORAs work, they’re hard to get. A month’s supply of naldemedine or methylnaltrexone can cost $500-$900 without insurance. Medicare Part D plans require prior authorization for 41% of prescriptions. Commercial insurers often force patients to try and fail on multiple laxatives before approving a PAMORA.
That’s called step therapy-and it’s killing people. A 2023 survey of 1,500 patients found that 57% stopped taking PAMORAs within six months-not because they didn’t work, but because they couldn’t afford them or the paperwork was too much.
Pharmacists are stepping in to help. Studies show that when pharmacists actively follow up with patients starting opioids, they increase the rate of appropriate laxative use by 43%. Ask your pharmacist to review your meds. They’re often the first to catch missed treatments.
What’s Next? The Future of OIC Management
By 2026, doctors may be able to predict who responds best to which treatment based on genetics. Early research suggests certain gene variants make people more sensitive to opioid effects in the gut. That could mean personalized treatment plans-no more trial and error.
There are also new combination pills in development: low-dose PAMORAs paired with osmotic laxatives. These could offer better results with fewer side effects.
But until then, the best advice remains simple: Don’t wait. Don’t suffer in silence. And don’t assume OTC laxatives are enough.
What You Can Do Today
If you’re on opioids and dealing with constipation, here’s your action plan:
- Start polyethylene glycol (PEG) daily-no waiting.
- Add a stimulant laxative like senna 2-3 times a week if PEG alone isn’t enough.
- Track your bowel movements using a simple journal: frequency, effort, stool consistency.
- Ask your doctor about the Bowel Function Index (BFI). A score above 30 means you need stronger treatment.
- If you’re still struggling after two weeks, request a referral to a gastroenterologist or pain specialist.
- Ask if a PAMORA is right for you-and if your insurance will cover it. If not, ask about patient assistance programs.
Chronic pain is hard enough. You shouldn’t have to add daily suffering from constipation on top of it. OIC is treatable. But only if you speak up-and act early.
Is opioid-induced constipation the same as regular constipation?
No. Regular constipation is often caused by diet, dehydration, or lack of movement. Opioid-induced constipation (OIC) happens because opioids directly slow gut movement by binding to receptors in the intestines. This means standard fixes like fiber or water often don’t work. OIC is persistent, doesn’t improve over time, and requires targeted treatments like PAMORAs.
Can I just use laxatives forever for OIC?
You can use osmotic laxatives like polyethylene glycol long-term safely. But stimulant laxatives should be limited to short-term use because they can cause dependency and damage the colon’s natural function over time. If you’re relying on stimulants for more than a few weeks, it’s a sign you need a stronger treatment like a PAMORA.
Do PAMORAs reduce pain relief?
No. PAMORAs are designed to block opioid effects only in the gut, not the brain. They don’t interfere with pain control. Studies confirm patients maintain the same level of pain relief while seeing major improvements in bowel function. That’s why they’re preferred over stopping opioids or reducing doses.
Why don’t doctors always talk about OIC?
Many doctors assume patients will mention constipation on their own. But patients often feel embarrassed or think it’s normal. A 2015 study found 78% of patients underestimated how serious OIC would be. Doctors also face time constraints and may not be up to date on guidelines. It’s up to you to bring it up-especially when starting opioids.
Is there a test to diagnose OIC?
There’s no single blood test or scan. Diagnosis is based on symptoms and timing-constipation that started after beginning opioid therapy. Doctors may use the Bowel Function Index (BFI), a simple questionnaire scored out of 100. A score above 30 confirms clinically significant constipation requiring treatment. Imaging may be used if obstruction is suspected.
Can I switch to a different pain medication to avoid OIC?
Some non-opioid options like gabapentin, duloxetine, or physical therapy can help with certain types of pain. But for severe, chronic pain, opioids are often still necessary. Switching isn’t always possible or safe. The goal isn’t to stop opioids-it’s to treat OIC while keeping you pain-free.
How long does it take for PAMORAs to work?
It depends on the drug. Methylnaltrexone (Relistor®) injections work in 30 minutes to 4 hours. Naldemedine (Movantik®) pills usually take 24-48 hours. Lubiprostone (Amitiza®) may take up to a week for full effect. Don’t expect instant results with pills-but injections can be life-saving in emergencies.
Are there natural remedies that help with OIC?
Exercise, hydration, and fiber can help a little-but they won’t fix the core problem. Opioids override the body’s natural bowel signals. No amount of prunes, flaxseed, or yoga will reverse the chemical blockade. These can support treatment but should never replace it. Relying on them alone often leads to worsening symptoms.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.