When you’re managing type 2 diabetes, choosing the right medication isn’t just about lowering blood sugar-it’s about finding something that fits your life, your body, and your long-term health goals. Three of the most common oral (or taken by mouth) diabetes medications are metformin, sulfonylureas, and GLP-1 agonists. But they work in very different ways, come with very different risks, and affect your weight, energy, and even your heart in ways you might not expect.
Metformin: The Long-Standing Starter
Metformin has been the go-to first-line treatment for type 2 diabetes for over two decades. It’s cheap, widely available, and has a solid safety record. Originally developed in the 1920s, it wasn’t approved in the U.S. until 1995, but since then, it’s been prescribed over 92 million times a year in the U.S. alone.
How does it work? It doesn’t make your body produce more insulin. Instead, it tells your liver to stop dumping extra glucose into your bloodstream and helps your muscles use insulin more effectively. That means it lowers blood sugar without causing low blood sugar-unlike some other drugs.
Most people take 500 to 1,000 mg twice a day, usually with meals. The biggest downside? Up to 30% of users get stomach issues-diarrhea, nausea, bloating. Many switch to the extended-release version (Metformin ER) to cut those side effects. Some people still can’t tolerate it, no matter the brand or dose.
On average, metformin lowers A1C by 1% to 2%. It doesn’t cause weight gain-most people lose 2 to 3 kg over time. It’s also linked to lower heart disease risk, though not as strongly as newer drugs. One 2024 study of over 2.5 million patients found metformin users had more than double the odds of being diagnosed with Alzheimer’s compared to those on GLP-1 agonists, though the reason isn’t clear yet.
Sulfonylureas: The Old Guard With Hidden Costs
Sulfonylureas like glipizide (Glucotrol) and glimepiride (Amaryl) were the first oral diabetes pills ever made. They hit the market in the 1950s after scientists accidentally discovered their blood-sugar-lowering effect while studying antibiotics.
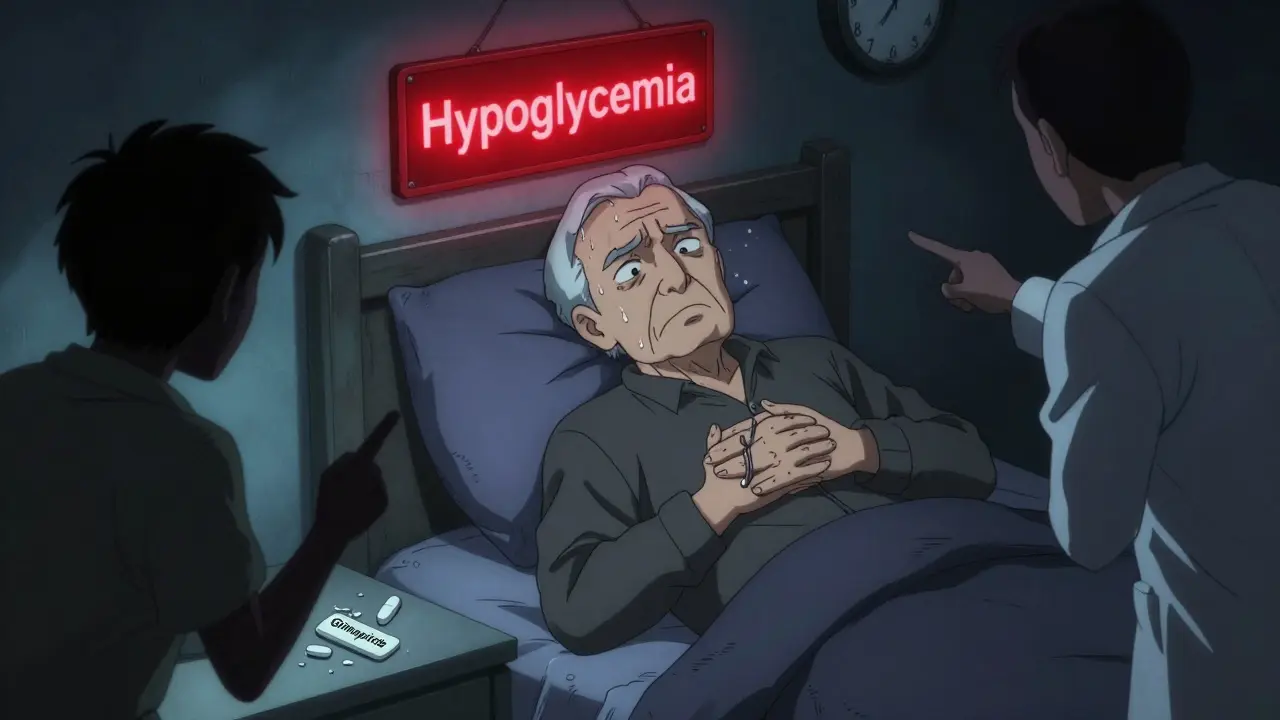
These drugs force your pancreas to pump out more insulin, no matter what your blood sugar is. That’s why they work quickly-but also why they’re risky. If you skip a meal, exercise more than usual, or drink alcohol, your blood sugar can crash. About 15% to 30% of users have mild to moderate low blood sugar each year. Around 2% to 4% end up in the ER because of severe hypoglycemia.
They lower A1C by about 1% to 1.5%, similar to metformin. But here’s the catch: they cause weight gain-typically 2 to 4 kg. That’s the opposite of what most people with type 2 diabetes need. They also don’t protect your heart. In fact, some studies suggest they might be worse for cardiovascular health than metformin.
Patients on sulfonylureas often need to check their blood sugar 2 to 3 times a week just to catch silent lows. Many doctors now avoid prescribing them as first-line, especially for older adults or those with irregular eating habits. Still, they’re used because they’re cheap-$10 to $30 a month without insurance.
GLP-1 Agonists: The New Powerhouse (Yes, Even the Oral Ones)
GLP-1 agonists are a game-changer. Originally developed after scientists discovered the body’s natural “incretin” system in the 1960s, these drugs mimic a hormone your gut releases after eating. They help your pancreas make insulin only when blood sugar is high, slow digestion, and reduce appetite.
For years, they came as daily or weekly injections-like liraglutide (Victoza) and semaglutide (Ozempic). But in 2019, the FDA approved oral semaglutide (Rybelsus), the first pill form. Real-world data shows 78% of people stick with the pill version, compared to just 62% with injections.
They lower A1C by 0.8% to 1.5%, slightly less than metformin on average-but they also help you lose weight. Most users drop 3 to 6 kg, sometimes more. One patient on Reddit reported losing 18 pounds in three months on Ozempic without changing their diet.
But they come with trade-offs. Up to 40% of users get nausea, vomiting, or diarrhea, especially when starting or increasing the dose. Slow titration helps-most doctors bump the dose every 4 weeks. The good news? These side effects usually fade after a few months.
And here’s the biggest win: GLP-1 agonists protect your heart. The LEADER trial showed liraglutide cut major heart events by 13%. They also lower the risk of kidney disease and liver problems. That’s why the American Diabetes Association now recommends them as second-line for anyone with heart disease, kidney disease, or high risk.
Cost is the biggest barrier. Without insurance, oral semaglutide runs $700 to $900 a month. Injectable versions cost the same. That’s why many patients stay on metformin or sulfonylureas-even if they’re less effective or riskier.
Head-to-Head: What the Numbers Really Show
Let’s compare these three drugs side by side, based on real-world studies and clinical trials:
| Feature | Metformin | Sulfonylureas | GLP-1 Agonists |
|---|---|---|---|
| A1C Reduction | 1.0%-2.0% | 1.0%-1.5% | 0.8%-1.5% |
| Weight Effect | Neutral to -3 kg | +2 to +4 kg | -3 to -6 kg |
| Hypoglycemia Risk | Very low | High (15-30% per year) | Very low |
| Cardiovascular Benefit | Mild | Neutral or negative | Strong (13% lower events) |
| Common Side Effects | Diarrhea, nausea (20-30%) | Hypoglycemia, weight gain | Nausea, vomiting (20-40%) |
| Cost (monthly, no insurance) | $4-$10 | $10-$30 | $700-$900 |
| Dosing Frequency | 1-2 times daily | 1-2 times daily | Once daily (oral) or weekly (injectable) |
The data is clear: GLP-1 agonists outperform sulfonylureas in nearly every category-except price. Even compared to metformin, they offer better weight loss and heart protection. But metformin still wins on safety, cost, and simplicity.
Who Gets What? Real-World Prescribing Trends
In 2023, metformin was still the most prescribed diabetes drug in the U.S. But GLP-1 agonists are catching up fast. Semaglutide (Ozempic) became the third most prescribed diabetes medication that year, beating out sulfonylureas.
Doctors are shifting. Among patients needing a second drug after metformin, 35% now get a GLP-1 agonist. Only 25% get a sulfonylurea. Why? Because guidelines changed. The American Diabetes Association now says: if you have heart disease, kidney disease, or obesity, start with a GLP-1 agonist-even before sulfonylureas.
But access isn’t equal. In Australia, where I live, public prescription subsidies cover metformin and sulfonylureas fully. GLP-1 agonists are only subsidized for patients with very high A1C or existing complications. Many patients pay out of pocket-or go without.
What Patients Are Saying
Real people tell the real story:
- “Metformin gave me constant diarrhea-even the extended-release version. I tried every brand. I switched to Ozempic and now I feel like I’ve got my life back.” - Reddit user, 2023
- “I had four ER visits from low blood sugar on glipizide. I thought it was just bad luck. Turns out, it’s the drug.” - HealthUnlocked user, 2023
- “I was on metformin for 10 years. My A1C was 7.8. After 6 months on Rybelsus, it’s 5.9. I lost 22 pounds. My doctor said I’m in remission.” - ADA Community, 2023
These aren’t outliers. A Drugs.com survey of 1,200 users showed GLP-1 agonists had the highest effectiveness rating (68%) and overall satisfaction (7.2/10), despite nausea. Metformin scored lower on satisfaction (6.5/10) because of side effects. Sulfonylureas were rated lowest for safety.
What to Do Next
If you’re just starting diabetes meds, metformin is still the safest, cheapest bet. But if you’ve got heart disease, obesity, or trouble staying on track with diet and exercise, talk to your doctor about GLP-1 agonists-even the pill form.
If you’re already on sulfonylureas and getting low blood sugar, or gaining weight, it’s time to revisit your plan. Switching to a GLP-1 agonist or SGLT-2 inhibitor could be life-changing.
Don’t let cost stop you. Many manufacturers offer copay cards. Novo Nordisk’s Care Connections program can bring Ozempic’s cost down to $0 for eligible patients. Ask your pharmacist. Ask your doctor. Don’t assume it’s out of reach.
The future of diabetes treatment isn’t about one-size-fits-all pills. It’s about matching the drug to the person-your weight, your heart, your budget, your tolerance for side effects. The tools are better than ever. It’s just a matter of choosing the right one.
Can you take metformin and GLP-1 agonists together?
Yes, and it’s very common. Many people start with metformin and add a GLP-1 agonist if their A1C doesn’t reach target. Combining them gives better blood sugar control than either alone, with less weight gain and lower hypoglycemia risk than adding sulfonylureas. Studies show the combo lowers A1C by about 1.5% on average.
Why are GLP-1 agonists so expensive?
They’re biologic drugs, meaning they’re made from living cells, not chemically synthesized like metformin. Manufacturing is complex, and patents protect them from cheaper generics. However, biosimilars are in development and could cut prices by 60-80% within the next 3-5 years. Some manufacturers offer patient assistance programs that reduce costs to $0 for qualifying users.
Do GLP-1 agonists cause pancreatitis or thyroid cancer?
Animal studies showed a link to thyroid tumors, so these drugs carry a black box warning against use in people with a personal or family history of medullary thyroid cancer. Human studies haven’t confirmed a clear risk, but doctors avoid them in high-risk patients. Pancreatitis risk is very low-less than 1 in 1,000 users-and mostly seen in those with prior pancreas issues.
Is metformin safe for people with kidney problems?
It depends. Metformin used to be avoided in anyone with kidney issues, but guidelines changed in 2022. You can take it safely if your eGFR is above 45. Between 30 and 45, use a lower dose. Below 30, it’s not recommended due to lactic acidosis risk. Always get your kidney function checked before starting and yearly after.
What’s the difference between oral and injectable GLP-1 agonists?
Oral semaglutide (Rybelsus) is absorbed through the gut with a special enhancer that helps it cross into the bloodstream. It’s taken once daily on an empty stomach. Injectable versions (like Ozempic) are absorbed under the skin and last longer-once weekly. Both work similarly, but the pill has slightly lower A1C reduction and more stomach upset. The pill’s big advantage is convenience-no needles.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.