Every year, over 90% of prescriptions in the U.S. are filled with generic drugs. They’re cheaper, just as effective for most people, and save the system billions. But sometimes, a doctor steps in and says: no generics. Not this time. This patient gets the brand name. That’s a prescriber override-and it’s not a loophole. It’s a legally protected clinical decision, buried in state laws, pharmacy systems, and electronic prescriptions.
Why Do Doctors Override Generic Substitution?
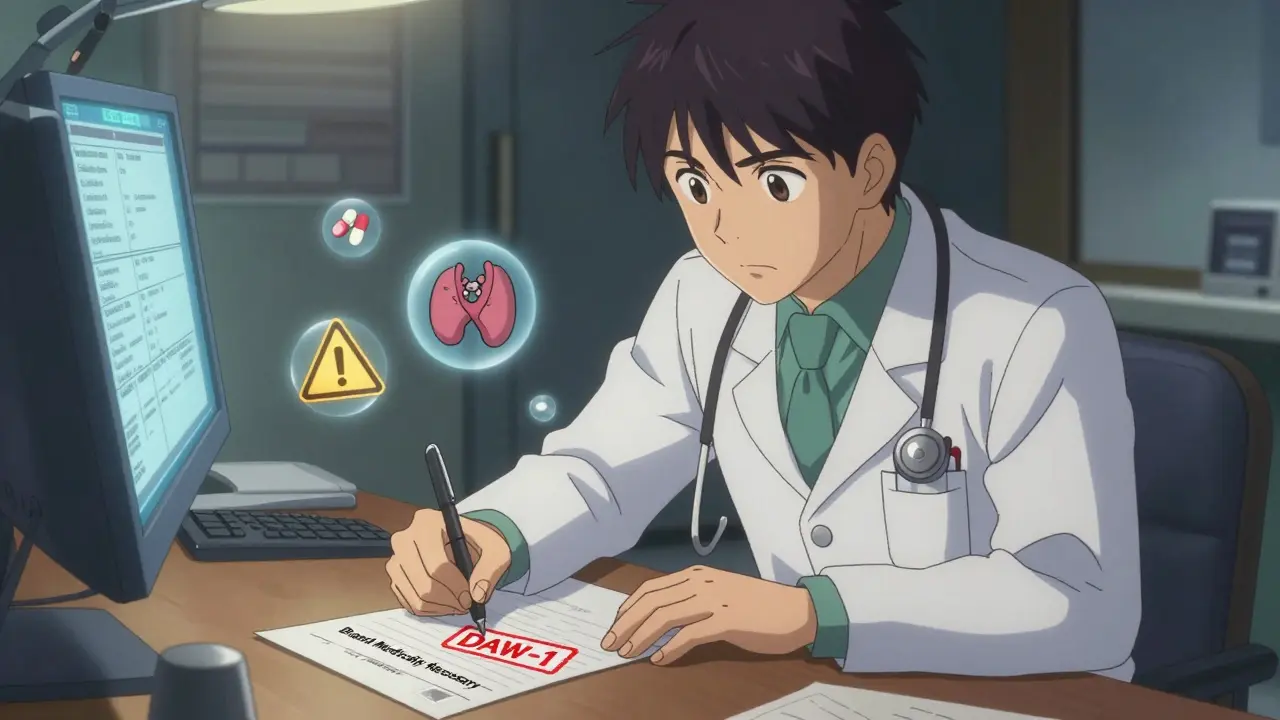
Generic drugs aren’t just cheaper versions of brand-name drugs. They’re required by the FDA to have the same active ingredient, strength, dosage form, and route of administration. So why wouldn’t a doctor just let the pharmacist swap them out? Because for some drugs, even tiny differences matter. Take levothyroxine, the most common treatment for hypothyroidism. Two generics might both contain levothyroxine sodium-but different fillers, dyes, or manufacturing processes can change how much of the drug gets absorbed. For a patient stabilized on one brand, switching to a generic-even one rated "A" in the FDA’s Orange Book-can cause their TSH levels to spike or crash. That’s not theoretical. In 2021, the Institute for Safe Medication Practices documented 27 serious adverse events linked to inappropriate substitutions of levothyroxine, warfarin, or phenytoin. Other drugs with narrow therapeutic indexes-like seizure medications (phenytoin, carbamazepine), blood thinners (warfarin), and some psychiatric drugs (lithium, valproate)-have very little room for error. A 5% change in absorption can mean the difference between control and crisis. Patients with documented allergies to inactive ingredients in generics-like lactose, dyes, or gluten-are another group where overrides are medically necessary. And some patients have tried generics before, had therapeutic failure, and seen symptoms return. That’s not anecdotal. It’s clinical evidence.How Does a Prescriber Override Actually Work?
It doesn’t happen by shouting at the pharmacist. It happens through a code: DAW-1. DAW stands for "Dispense As Written." DAW-1 means: "The prescriber has explicitly said no substitution is allowed." This code is part of the NCPDP Telecommunications Standard, used by every e-prescribing system in the U.S. But here’s the catch: every state has its own rules about how that code gets written. - In Illinois, the prescriber must check a box labeled "May Not Substitute" on the prescription form. - In Kentucky, they must write "Brand Medically Necessary" by hand. - In Massachusetts, "No Substitution" is enough. - In Michigan, it has to say "DAW" or "Dispense as Written," handwritten. - In Oregon, the prescriber can say it verbally, in writing, or electronically-but they can’t just pick a default option in the EHR. If the notation doesn’t match the state’s exact requirement, the pharmacy system will often default to substitution anyway. And that’s where things go wrong. A 2022 survey of 1,247 physicians on Sermo found that 41% said their electronic health record templates didn’t match their state’s override rules. One doctor in Texas wrote "Do Not Substitute"-but Texas law requires "Brand Medically Necessary." The pharmacy processed it as a generic. The patient had a seizure.The Cost of Override: Why Payers Care
Generic drugs saved the U.S. healthcare system $2.2 trillion between 2010 and 2019. That’s why insurers and pharmacy benefit managers (PBMs) watch DAW-1 usage closely. On average, a DAW-1 prescription costs 32.7% more than a substituted generic. For drugs like Humira or Enbrel, that’s hundreds of dollars per month. In 2021, Express Scripts reported that 18.4% of avoidable brand-drug spending came from inappropriate DAW-1 designations. The American Pharmacists Association estimates that 5-7% of all prescriptions might legitimately need an override. But studies show physicians are overusing them. A 2010 survey found only 58.3% of doctors correctly understood their own state’s override rules. And 22.7% admitted they’d accidentally allowed substitutions because of documentation errors. Dr. William Shrank, Chief Scientific Officer at UnitedHealth Group, says many physicians overestimate the clinical risk of switching to generics. "Minor formulation differences rarely matter," he says. "But when they do, it’s critical. The problem is we don’t always know which is which."
What Happens When the Override Fails?
The system is designed to catch errors-but it doesn’t always. Pharmacists are supposed to check the FDA’s Orange Book before substituting. That’s the official list of drugs rated as therapeutically equivalent. If a drug has an "A" rating, substitution is allowed unless overridden. But if the prescriber’s override isn’t clear? The pharmacist might assume it’s a mistake. Or the EHR might auto-populate a generic. Or the pharmacy’s system might not recognize the handwritten notation. One Reddit user, "Dr_InternalMed," described a patient who was hospitalized for thyroid storm after a pharmacy substituted levothyroxine-even though the prescription had "DAW-1" written on it. The pharmacist said they didn’t recognize the notation because it wasn’t in their system’s approved list. These aren’t rare. Between 2018 and 2022, the Institute for Safe Medication Practices recorded 27 serious adverse events tied to failed overrides on narrow therapeutic index drugs.How to Get It Right: A Practical Guide for Doctors
If you need to override a generic, here’s how to make sure it sticks:- Know your state’s exact wording. Don’t guess. Check your state pharmacy board’s website. The National Association of Boards of Pharmacy has an interactive map updated quarterly.
- Use your EHR’s override template-but verify it. Many EHRs have default settings that auto-select "Dispense as Generic." Turn that off. Customize your template to match your state’s requirement.
- Don’t rely on "Do Not Substitute." That phrase isn’t legally recognized in many states. Use the exact language your state requires.
- Document the reason. Even if your state doesn’t require it, write "History of therapeutic failure with generic" or "Allergic to dye in generic" next to the DAW-1 code. It helps pharmacists understand the urgency.
- Check if your patient’s insurance requires prior authorization. Many Medicare Part D and commercial plans automatically flag DAW-1 prescriptions for review. If you don’t submit supporting documentation, the claim gets denied-and the patient gets the generic anyway.
What’s Changing? The Future of Prescriber Override
The system is slowly getting smarter. In 2023, the FDA released Orange Book version 4.0, which now includes biosimilar interchangeability codes. That will soon affect overrides for biologics like insulin and rheumatoid arthritis drugs. The NCPDP plans to embed state-specific override rules directly into the SCRIPT 201905 e-prescribing standard by Q3 2024. That means your EHR will auto-populate the correct wording based on your location and the patient’s pharmacy. A federal bill, the Standardized Prescriber Override Protocol Act, was introduced in Congress in 2023. It wouldn’t ban overrides-it would standardize them. One code. One format. One rule across all 50 states. Until then, the patchwork remains. And the burden falls on doctors to know the rules, use them correctly, and protect their patients from preventable harm.When Override Isn’t the Answer
Just because you can override doesn’t mean you should. For 90% of prescriptions, generics are safe, effective, and the right choice. Overriding without a clear clinical reason isn’t just wasteful-it’s risky. It undermines the system designed to keep costs down and access high. If a patient is stable on a generic, don’t switch them to a brand unless there’s documented failure. If a patient is new to therapy, start with the generic. If they have a reaction, then document it. Then override. The goal isn’t to prevent substitution. It’s to ensure it doesn’t happen when it could hurt someone.Can a pharmacist override a prescriber’s DAW-1 request?
No. If a prescriber properly documents DAW-1 according to state law, the pharmacist is legally required to dispense the brand-name drug. Refusing to do so is a violation of pharmacy regulations and could result in disciplinary action. The only exception is if the brand is unavailable-but even then, the pharmacist must notify the prescriber and document the reason.
Do all states require the same wording for a prescriber override?
No. Each state has its own legal requirements for how a prescriber must indicate that substitution is not allowed. Some require a checkbox, others require handwritten phrases like "Brand Medically Necessary" or "DAW." Using the wrong wording-even if you meant to override-can result in the pharmacy dispensing a generic. Always check your state’s pharmacy board guidelines.
What’s the difference between DAW-1 and DAW-2?
DAW-1 means the prescriber has mandated no substitution. DAW-2 means the patient requested the brand-name drug, even though a generic is available. In DAW-2 cases, the patient pays the difference in price. In DAW-1, the prescriber’s order overrides cost considerations entirely.
Can a prescriber override be done electronically?
Yes, in most states. Electronic prescribing systems can transmit DAW-1 codes directly to pharmacies. However, some states still require handwritten notation on paper prescriptions, even if the original was sent electronically. Always verify your state’s rules-some require both electronic and written documentation.
Why do some pharmacies reject DAW-1 requests?
Common reasons include: unclear or non-standard wording on the prescription, missing prescriber signature, EHR templates that don’t match state requirements, or insurance systems that auto-denied the override due to lack of prior authorization. If a pharmacy rejects a DAW-1, ask them to explain why-and document their response. You may need to call them directly or resubmit with corrected notation.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.