SSRI & Opioid Safety Checker
Important Note: This tool provides general information only. Always consult your doctor or pharmacist before changing your medication regimen.
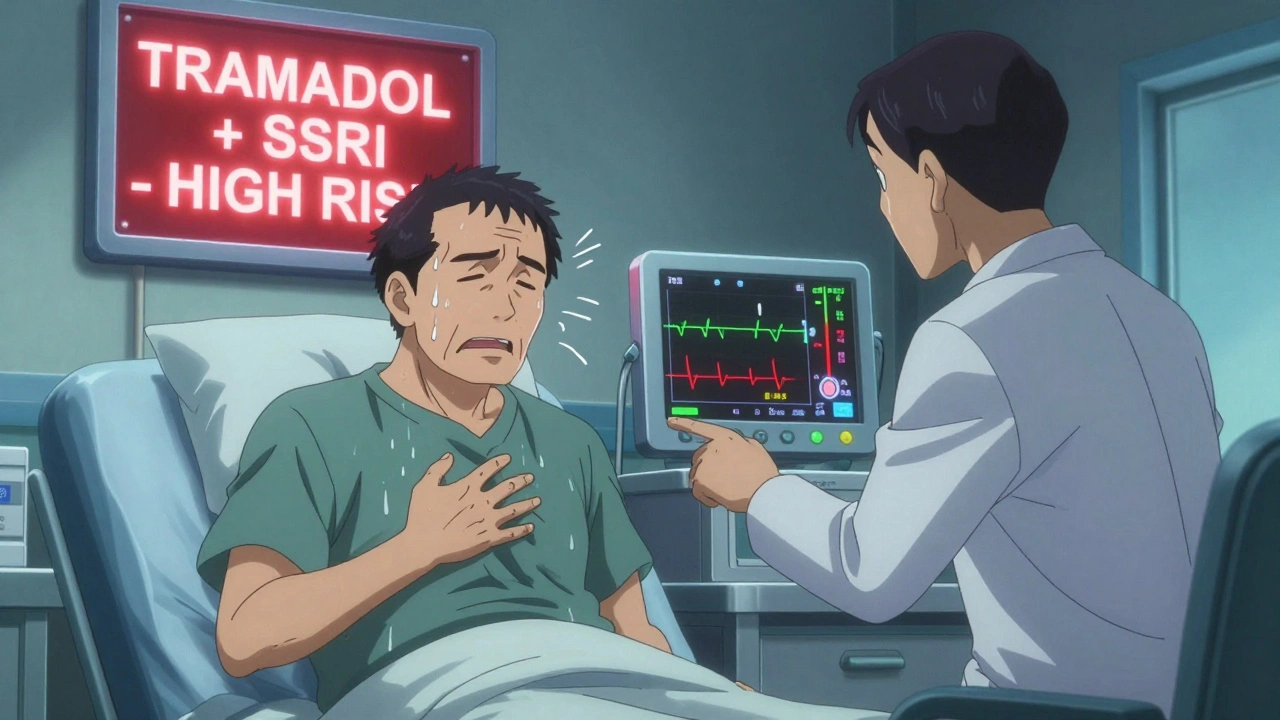
When you’re taking an SSRI for depression or anxiety, and your doctor adds an opioid for pain, it’s easy to assume both are safe together. But that’s not always true. The real danger isn’t just side effects-it’s serotonin syndrome, a rare but life-threatening reaction that can strike within hours. It doesn’t happen often, but when it does, it’s often missed-mistaken for a fever, a panic attack, or even a drug overdose. And the most common trigger? A combination of an SSRI and certain opioids, especially tramadol.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t an allergy. It’s a toxic buildup of serotonin in your brain and nervous system. Serotonin is a natural chemical that helps regulate mood, sleep, and pain. But when too much of it floods your system-usually because two drugs are boosting it at once-your nerves get overstimulated. Think of it like a circuit breaker tripping from too much current. Symptoms start mild: shivering, sweating, a racing heart, or restless legs. But they can escalate fast. Muscle rigidity, high fever (over 41°C), seizures, confusion, and even unconsciousness can follow. Without quick treatment, it can be fatal. Emergency departments see about 1 in 7 cases of serotonin overdose turn serious. And here’s the kicker: nearly half of these cases are misdiagnosed at first.Which Opioids Are Safe With SSRIs?
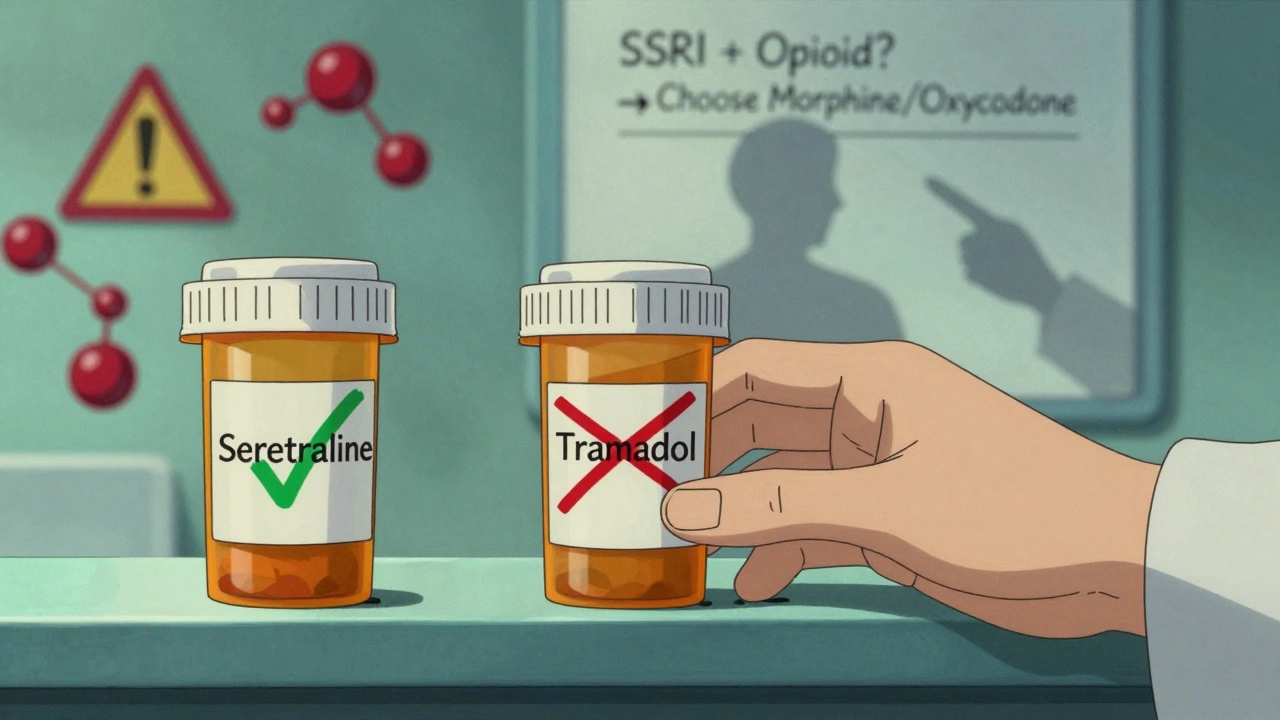
Not all opioids are created equal when it comes to serotonin. Some barely touch it. Others are basically serotonin boosters in disguise. High-risk opioids:- Tramadol - This one’s the big one. It doesn’t just relieve pain; it blocks serotonin reuptake, just like an SSRI. Combine it with fluoxetine, sertraline, or escitalopram, and you’re doubling down on serotonin. Studies show tramadol-SSRI combos are over four times more likely to cause serotonin syndrome than morphine-SSRI combos.
- Methadone - Used for chronic pain or addiction treatment, methadone also inhibits serotonin reuptake. It’s less common than tramadol, but the risk is just as real.
- Pethidine (meperidine) - Rarely used today, but still found in some hospitals. High risk. Avoid it entirely if you’re on an SSRI.
- Morphine - Doesn’t affect serotonin reuptake. The go-to choice for pain relief in patients on SSRIs.
- Oxycodone - No significant serotonin activity. Safe for most people on antidepressants.
- Buprenorphine - Used for pain or opioid dependence. Minimal serotonin interaction.
- Hydromorphone - Similar to morphine. A good alternative if you need something stronger.
Which SSRIs Carry the Highest Risk?
Not all SSRIs are equal either. Their half-lives and how strongly they block serotonin reuptake matter a lot.- Fluoxetine (Prozac) - The worst offender. It sticks around for weeks. Even if you stop it, its active metabolite can linger for up to 16 days. That means if you switch to an opioid too soon after quitting fluoxetine, you’re still at risk.
- Sertraline (Zoloft) - Shorter half-life (about 26 hours). Lower risk than fluoxetine, but still dangerous with tramadol.
- Escitalopram (Lexapro), Paroxetine (Paxil) - Moderate risk. Paroxetine is a stronger serotonin blocker than others in its class.
Who’s Most at Risk?
It’s not just about the drugs. Your body matters too.- Older adults - People over 65 take more medications on average. They’re also more likely to have kidney or liver issues that slow drug clearance.
- People with liver or kidney disease - Your body can’t clear these drugs as quickly. Even normal doses can build up to toxic levels.
- Genetic poor metabolizers - About 7% of people have a gene variant (CYP2D6) that breaks down tramadol slowly. For them, even one dose can trigger serotonin syndrome.
- People recently starting or increasing doses - Most cases happen within 24 to 72 hours after a new drug is added or the dose is raised.
How to Prevent It
Prevention isn’t complicated. It’s about knowing the red flags and making smart choices.- Avoid high-risk combinations - If you’re on an SSRI or SNRI, don’t take tramadol, methadone, or pethidine. Period. Ask for morphine, oxycodone, or hydromorphone instead.
- Wait before switching - If you’re stopping fluoxetine, wait at least 5 weeks before starting an opioid. For other SSRIs, wait 1 to 2 weeks. Don’t guess-ask your pharmacist.
- Start low, go slow - If you absolutely must combine a moderate-risk opioid with an SSRI, start at half the usual dose and watch closely for 72 hours.
- Use tech to your advantage - Many hospitals now have electronic alerts that block dangerous prescriptions. If your doctor prescribes tramadol while you’re on sertraline, ask: “Did the system flag this?”
- Know your symptoms - Keep this checklist handy: shivering you can’t stop, muscle twitching, fast heartbeat, sweating, confusion, or feeling like you’re burning up from inside. If you get any of these after starting a new pain med, stop it and call your doctor immediately.
What to Do If You Think You Have It
If serotonin syndrome is suspected, time is everything.- Stop all serotonergic drugs - Immediately. No exceptions.
- Call emergency services - Don’t wait. Go to the ER. Tell them you’re on an SSRI and an opioid.
- Don’t use antipsychotics - They can make it worse. Benzodiazepines like lorazepam are the first-line treatment to calm agitation and muscle rigidity.
- Severe cases need cyproheptadine - This is an antihistamine that blocks serotonin receptors. Doctors use it off-label for serious cases. Dosing: 12 mg initially, then 2 mg every 2 hours as needed.
- Lower your temperature - If you’re over 40°C, cooling blankets and ice packs are critical. Heat damage can kill you even if the serotonin levels drop.
Why This Is Getting Worse
Between 2017 and 2022, serotonin syndrome cases linked to opioids and antidepressants rose by 35%. Why? Tramadol prescriptions jumped. So did the number of people taking both antidepressants and painkillers. One in five opioid prescriptions now goes to someone already on an SSRI or SNRI. Regulators are catching on. The FDA added stronger warnings to tramadol labels in 2022. The European Medicines Agency did the same. Kaiser Permanente cut dangerous tramadol-SSRI prescriptions by 87% just by adding a computer alert. But the real problem? Many doctors still don’t know the risks. A hospital pharmacist in Perth told me they see 2-3 cases a month. All from tramadol and SSRIs. All preventable.Bottom Line
You don’t have to choose between pain relief and mental health care. But you do need to be smart about how you combine them. Tramadol is not your friend if you’re on an SSRI. Morphine or oxycodone are safer. Fluoxetine is riskier than sertraline. Waiting after stopping an SSRI isn’t optional-it’s life-saving. If you’re on an SSRI and your doctor suggests an opioid, ask: “Is this one safe with my antidepressant?” If they say yes without checking, ask again. If they can’t answer, get a second opinion. Your life might depend on it.Can you get serotonin syndrome from just one drug?
Rarely. Serotonin syndrome almost always happens when two or more serotonergic drugs are combined. Overdosing on a single SSRI can cause it, but it’s uncommon. Most cases involve a drug interaction-like an SSRI plus tramadol or methadone.
Is it safe to take codeine with an SSRI?
It’s usually considered low risk, but not zero. There are documented cases of serotonin syndrome with codeine and SSRIs, especially in people who metabolize codeine unusually fast or slow. If you’ve never had issues before, it may be fine. But if you develop shivering, agitation, or rapid heartbeat after starting codeine, stop it and get help.
How long should I wait after stopping an SSRI before taking an opioid?
It depends on the SSRI. For fluoxetine, wait 5 weeks because it stays in your system so long. For sertraline, escitalopram, or citalopram, wait at least 1 to 2 weeks. For paroxetine, wait 2 weeks. Don’t guess-ask your pharmacist or doctor for the exact timeline based on your specific medication.
Can serotonin syndrome be treated at home?
No. Mild cases might seem manageable, but symptoms can worsen rapidly. Even if you feel okay now, your temperature or heart rate could spike in the next few hours. Serotonin syndrome requires medical supervision. Call emergency services or go to the ER if you suspect it.
Are there any new tools to help prevent this?
Yes. Hospitals are adding automated alerts in their electronic systems to block dangerous combinations like tramadol with SSRIs. Some systems now check your genetics too-like whether you’re a poor metabolizer of CYP2D6, which increases risk. In 2024, major EHR platforms like Epic will roll out more advanced risk assessments that look at 17 different gene-drug interactions related to serotonin.
What should I ask my doctor before starting a new opioid?
Ask: ‘Is this opioid safe to take with my current antidepressant?’ and ‘Is there a safer alternative?’ If they say ‘yes’ without checking, ask for the evidence. Also ask: ‘What symptoms should I watch for?’ and ‘What do I do if I feel unwell?’ Don’t assume they know the interaction-many don’t.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.