Elderly Drug Safety: Protecting Seniors from Dangerous Medication Risks
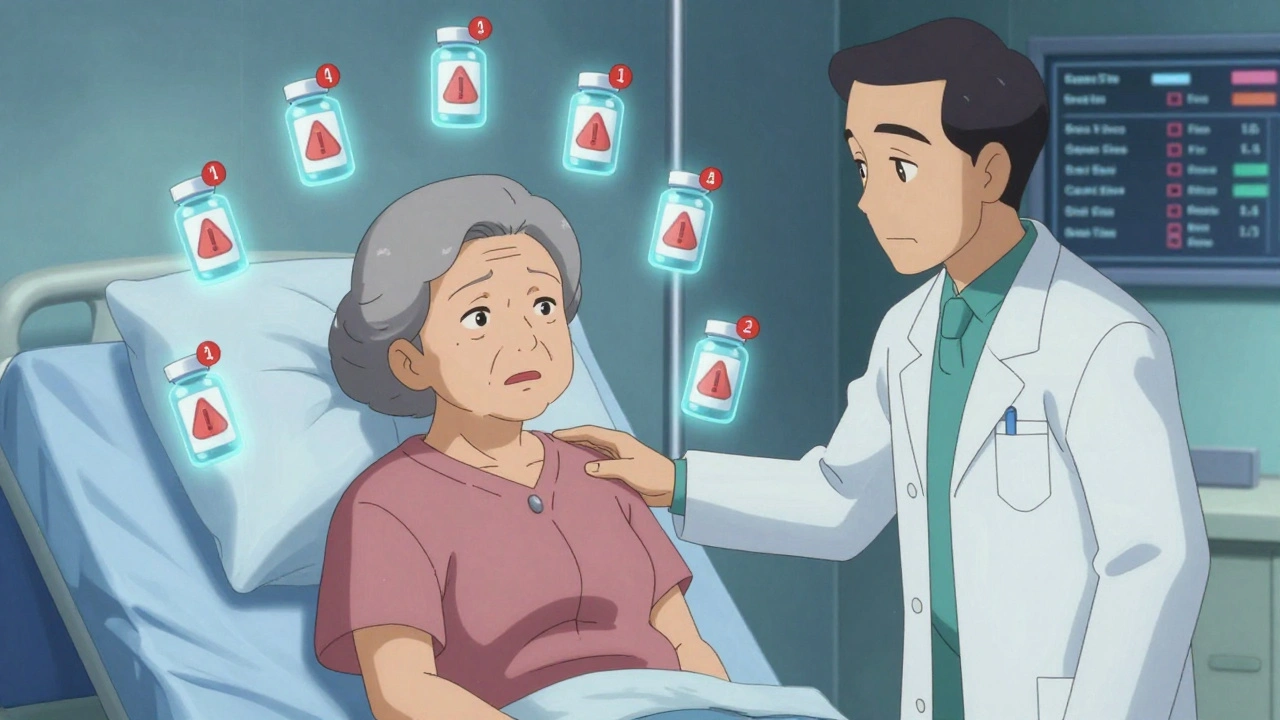
When it comes to elderly drug safety, the careful use of medications in older adults to prevent harm from side effects, interactions, and improper dosing. Also known as senior medication safety, it’s not just about giving the right pill—it’s about knowing which pills shouldn’t be mixed, how aging changes the body’s response, and why what works for a 40-year-old can be deadly for a 75-year-old. The average senior takes four to five prescription drugs daily. Add over-the-counter meds, supplements, and herbal remedies, and that number can jump to ten or more. This is called polypharmacy, the use of multiple medications by a patient, often leading to increased risk of adverse effects. Also known as multiple drug use, it’s one of the biggest hidden dangers in geriatric care. A single interaction—like mixing a common painkiller with a blood thinner—can send someone to the ER. And it’s not rare. The FDA reports that over 100,000 older adults are hospitalized each year just from medication-related problems.
Why does this happen? Aging changes how the body handles drugs. Kidneys and liver slow down, so medications stick around longer. Stomach acid drops, changing how pills are absorbed. Muscle mass shrinks, fat increases—this alters how drugs are distributed. A dose that was fine at 60 might be toxic at 80. And many seniors don’t know their own meds. They might take two pills with the same active ingredient because they look different. Or skip doses because they’re confused by the schedule. Some even reuse old prescriptions when symptoms return, not realizing the cause changed.
That’s why understanding medication interactions, how two or more drugs affect each other’s behavior in the body, often leading to dangerous side effects. Also known as drug-drug interactions, these are the silent killers in nursing homes and living rooms alike. A cough syrup with dextromethorphan can trigger serotonin syndrome when taken with an SSRI. Grapefruit juice can turn a statin into a muscle-damaging toxin. Even common antacids can block absorption of antibiotics or thyroid meds. And it’s not just pills. Patches, inhalers, and injections all behave differently in older bodies. The FDA’s FAERS reports, a public database of adverse drug reactions submitted by patients and providers. Also known as FDA Adverse Event Reporting System, this system shows that seniors are overrepresented in reports of serious side effects—not because they’re more sensitive by nature, but because their medication regimens are more complex.
There’s no magic bullet. But there are practical steps. Always keep a current list of every pill, patch, and supplement. Bring it to every doctor visit. Ask: "Is this still needed?" and "Could this interact with anything else I take?" Pharmacists are your best allies—they see all the meds at once. Don’t assume a generic is always safe; even small changes in formulation can affect seniors differently. And never ignore a new symptom—dizziness, confusion, nausea, or a fall—without asking if it could be a drug reaction.
What follows is a collection of real, practical guides written for people who care about elderly drug safety. You’ll find deep dives into how generics behave in older bodies, how to spot fake pills, how to read warning labels, and what to do when medications don’t just stop working—they start hurting. These aren’t theory pieces. They’re tools for protecting someone you love. Read them. Use them. Share them.