Obesity and Sleep Apnea: How Excess Weight Disrupts Breathing at Night
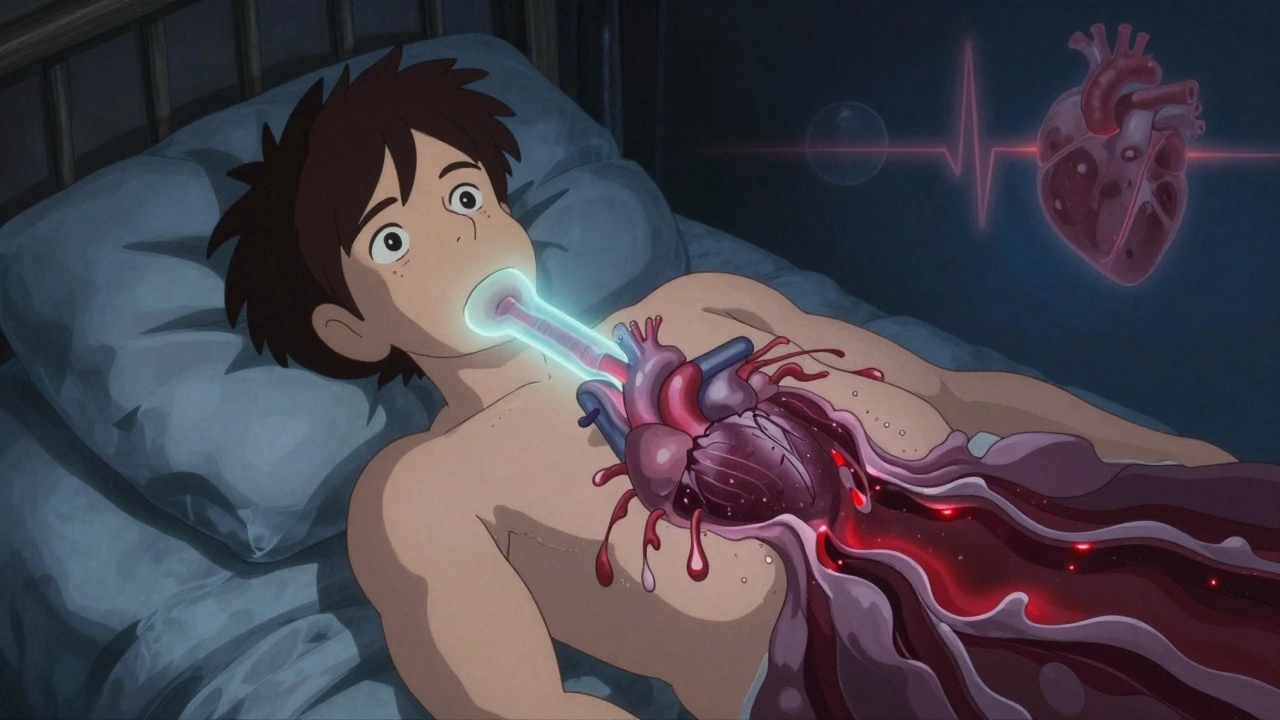
When you carry extra weight, especially around your neck and belly, it doesn’t just change how your clothes fit—it changes how you breathe while sleeping. Obesity and sleep apnea, a condition where breathing repeatedly stops and starts during sleep due to blocked airways. This isn’t just snoring—it’s a medical issue that increases your risk of heart attack, stroke, and type 2 diabetes. About 70% of people with obstructive sleep apnea are overweight or obese, and the more weight you carry, the tighter your airway gets when muscles relax at night.
Obstructive sleep apnea, the most common form of sleep apnea, happens when throat muscles collapse and block airflow. OSA isn’t caused by being lazy or not sleeping well—it’s a physical problem. Fat deposits around the neck squeeze the airway, and belly fat pushes up on the diaphragm, making it harder to take deep breaths. Even a 10% weight loss can cut apnea episodes in half for many people. That’s not a guess—it’s what multiple clinical studies have shown. And while CPAP machines help, they’re not a cure. If the weight stays, the problem comes back as soon as you stop using the device.
Weight loss and sleep apnea are connected in a way most people don’t expect. Losing weight doesn’t just reduce pressure on your airway—it also lowers inflammation, improves muscle tone, and helps your brain better control breathing during sleep. Some people see results after dropping just 10 to 15 pounds. Others need more. But the pattern is clear: the scale moves, the breathing improves. Surgery like gastric bypass can resolve sleep apnea in over 80% of cases, not because it removes fat from the neck, but because it resets how the body regulates energy and breathing. And here’s the thing—many doctors still don’t screen obese patients for sleep apnea unless they’re loud snorers. But quiet sleepers with daytime fatigue, high blood pressure, or trouble concentrating? They’re just as at risk.
That’s why the posts here focus on real, evidence-based connections between weight, breathing, and medication safety. You’ll find guides on how certain drugs affect weight gain or sleep quality, what to ask your doctor if you’re on blood pressure meds and struggling with fatigue, and how to spot hidden risks when combining sleep aids with other prescriptions. This isn’t about quick fixes. It’s about understanding the system—how fat, airways, nerves, and meds interact—and making smarter choices based on what actually works.