Polypharmacy Risks: What Happens When You Take Too Many Medications
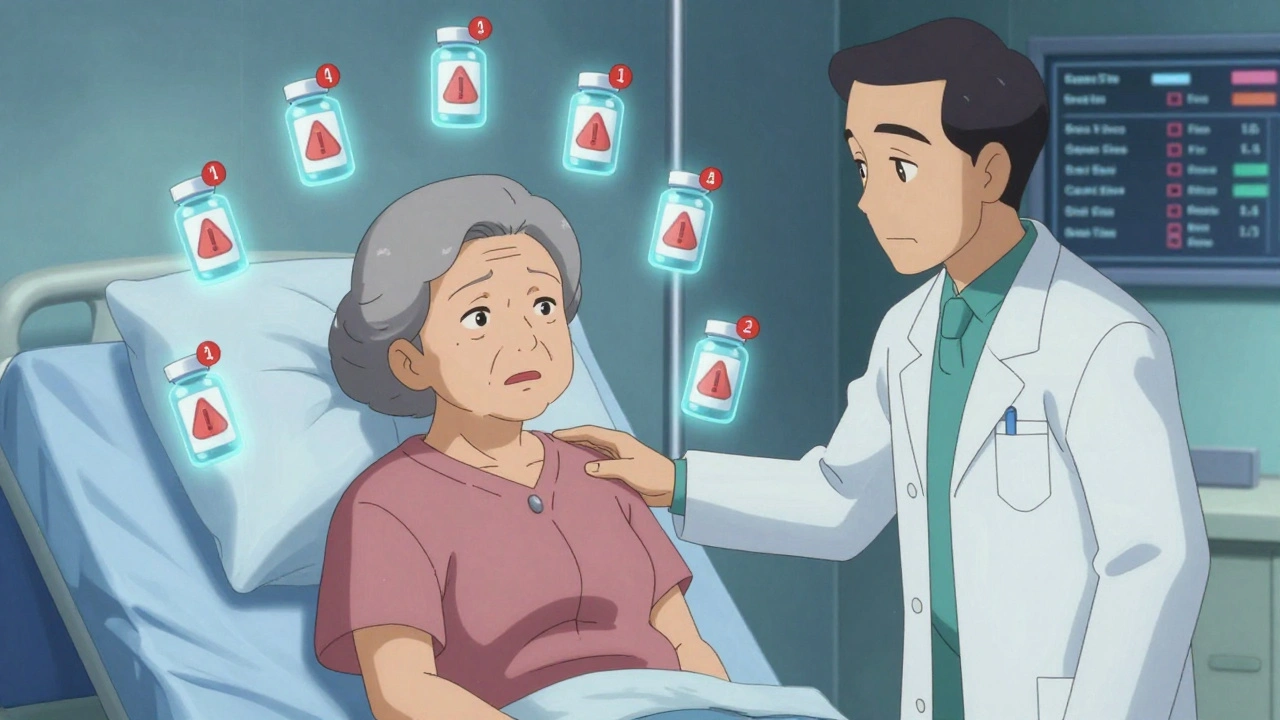
When you’re taking polypharmacy, the use of multiple medications by a single patient, often for different conditions. Also known as multiple medication use, it’s not uncommon—especially among older adults or those managing chronic illnesses. But what starts as necessary care can quickly turn into a hidden danger. The more pills you swallow, the higher the chance something will go wrong. It’s not just about side effects—it’s about how those drugs talk to each other inside your body.
Take drug interactions, when two or more medications change how each other works in your body. For example, mixing SSRIs with certain painkillers like tramadol can trigger serotonin syndrome—a fast-moving, life-threatening reaction. Or consider rifampin, a tuberculosis drug that turns off the effect of birth control, blood thinners, and even some antidepressants. These aren’t rare cases. They show up in FDA reports every day. And they’re not always obvious. Your doctor might not catch them unless you tell them everything you’re taking—even over-the-counter cough syrup or herbal supplements.
adverse drug reactions, harmful and unintended effects from medications are one of the top causes of hospital visits in people over 65. But it’s not just seniors. Anyone on five or more prescriptions is at risk. Think about it: if you’re on a statin, a blood pressure pill, an antidepressant, a painkiller, and a stomach acid reducer, that’s five chances for something to clash. And that’s before you add supplements like St. John’s Wort or grapefruit juice—which can turn a safe dose into a toxic one.
It’s easy to assume that if a doctor prescribed it, it’s safe. But doctors don’t always know everything you’re taking. Pharmacies don’t always flag every interaction. And sometimes, the real problem isn’t the drugs themselves—it’s how they pile up over time. One pill for sleep, another for anxiety, a third for joint pain, a fourth for heartburn. They’re all legal. They’re all prescribed. But together? They’re a ticking clock.
That’s why reading your prescription labels matters. That black box warning? It’s there for a reason. Skipping doses? That’s risky too—because inconsistent use can make interactions worse. And if you’re ever unsure, don’t guess. Ask your pharmacist. Bring a list of everything you take—every pill, patch, drop, and powder—to every appointment. You’d be surprised how many people forget their daily aspirin or their CBD oil.
The good news? You don’t have to live with this uncertainty. Many people can cut down on meds without losing control of their health. Sometimes, one pill can replace two. Sometimes, a lifestyle change can reduce the need for a drug altogether. And sometimes, just knowing the risks is the first step to avoiding them.
Below, you’ll find real-world examples of how these risks play out—from dangerous combos like opioids and benzodiazepines that slow your breathing, to cough medicines that trigger serotonin syndrome when mixed with antidepressants. These aren’t theoretical warnings. These are cases that led to ER visits, hospital stays, and worse. But they’re also cases where awareness made all the difference. What you’re about to read could help you—or someone you love—stay safe.