When you pick up a generic inhaler, patch, or injection, you expect it to work just like the brand-name version. But here’s the catch: these aren’t just pills with a different label. They’re complex machines delivering medicine in precise ways-into your lungs, through your skin, or straight into your bloodstream. Getting a generic version approved isn’t about matching active ingredients alone. It’s about proving the whole delivery system behaves the same way. That’s bioequivalence for special delivery systems, and it’s far more complicated than most people realize.
Why Bioequivalence Isn’t the Same for Inhalers, Patches, and Injections
For oral pills, bioequivalence is straightforward: measure how much drug hits your blood and how fast. If the generic’s AUC and Cmax fall within 80-125% of the brand, it’s approved. But that rule breaks down when the drug doesn’t need to enter your bloodstream at all.
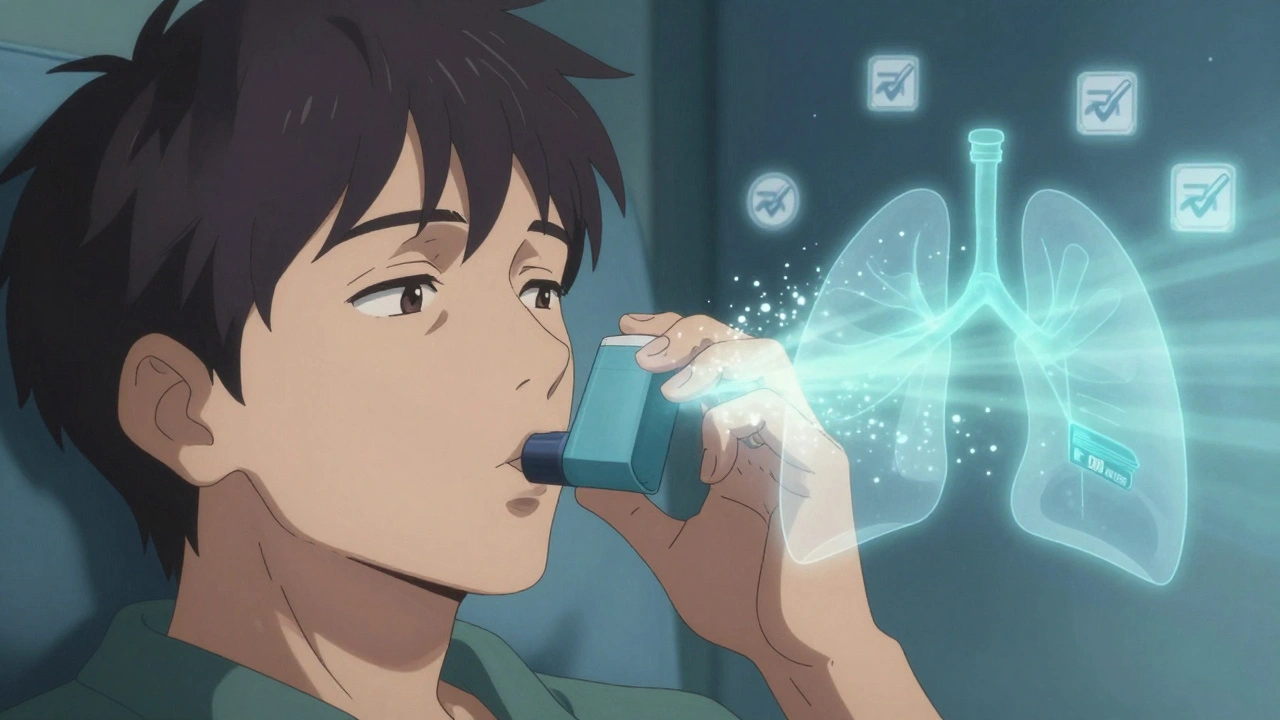
Take inhaled corticosteroids for asthma. The goal isn’t systemic absorption-it’s local action in the lungs. If a generic inhaler delivers the same amount of drug to your blood but only 60% of it reaches your airways, it’s useless. That’s why the FDA requires more than blood tests. They demand proof that the particle size is right (90% between 1 and 5 micrometers), the plume shape matches, and the dose per puff is consistent. Even a 2°C difference in plume temperature can trigger rejection, as one generic sponsor found out the hard way.
Transdermal patches are another story. These are designed to release drug slowly over hours or days. A generic patch might release 95% of its drug in 24 hours, but if it’s 10% slower in the first 6 hours, your pain relief won’t kick in on time. The FDA requires in vitro release profiles to match within 10% at every time point. Skin adhesion matters too-if the patch falls off early, the dose is lost.
Injectables like liposomal doxorubicin or enoxaparin (Lovenox) are even trickier. These aren’t simple solutions. They’re nanoparticles, micelles, or complex mixtures where size, charge, and structure determine how the drug behaves. For Lovenox, the FDA requires bioequivalence limits of 90-111% for AUC and Cmax-tighter than the usual 80-125%. Why? Because tiny changes in particle size can alter how the drug interacts with blood proteins, increasing bleeding risk.
The Testing Tools That Make or Break a Generic
Proving bioequivalence for these systems isn’t done in a standard lab. It needs specialized, expensive equipment.
For inhalers, scientists use cascade impactors-devices that capture drug particles at different air speeds to measure size distribution. A single instrument costs $150,000 to $300,000. They also test plume geometry with high-speed cameras and measure how much drug sticks to the mouthpiece. If your generic leaves 15% more residue than the brand, it’s rejected.
Transdermal patches are tested in Franz diffusion cells-glass chambers with human skin mounted between donor and receiver compartments. The patch sits on top; drug movement is measured over 24-72 hours. If the release rate dips below the brand’s curve at any point, even by 5%, it fails.
For injectables, laser diffraction and dynamic light scattering measure particle size. Zeta potential, which predicts stability, must match within 5 millivolts. Polydispersity index? Less than 0.2. Any deviation and the entire batch is suspect. These aren’t just guidelines-they’re hard limits.
And even then, some systems require live human testing. Scintigraphy imaging-where patients inhale a radioactive tracer and a camera tracks where the drug lands in the lungs-was key to approving Teva’s generic ProAir RespiClick. Without it, the FDA wouldn’t have been convinced.
Approval Rates and Why So Many Fail
Here’s the reality: 78% of standard oral generics get approved. For complex delivery systems? The numbers drop hard.
- Inhalers: 38% approval rate
- Transdermal patches: 52%
- Complex injectables: 58%
Why such a gap? Because the margin for error is razor-thin. A 2019 attempt to copy Advair Diskus failed not because of drug content-but because the fine particle fraction was 8% lower. That’s less than one puff out of twelve. The FDA rejected it anyway.
Another failure: a generic version of Bydureon BCise was pulled in 2021. The drug formula was fine. But the auto-injector mechanism delivered the dose slightly slower. That tiny delay changed the pharmacokinetic profile enough to trigger rejection. The sponsor lost $45 million.
These aren’t isolated cases. A 2022 survey of 127 generic drug developers found that 68% called bioequivalence requirements for complex products “excessively burdensome.” But 82% agreed they were necessary for safety. The trade-off is clear: higher costs and lower approval rates, but fewer patient risks.
The Cost and Time Burden
Developing a generic pill costs $5-10 million and takes 18-24 months. A generic inhaler? $25-40 million. And 36-48 months.
One formulation scientist spent $32 million and 42 months developing a generic insulin glargine. Why? Because the particle size distribution required 17 different formula tweaks. Each change meant new stability tests, new animal studies, new human trials. And that’s just one product.
These costs aren’t theoretical. They shape the market. Only 15% of the generic drug market by value comes from complex delivery systems-even though they make up 30% of prescriptions. Why? Because few companies can afford the risk. Only a handful of big players-Teva, Mylan, Sandoz-have the resources to navigate this maze. Smaller firms often give up before they start.
How the Industry Is Adapting
Regulators aren’t standing still. The FDA, EMA, and WHO have all released product-specific guidance. The FDA’s 2023 draft guidance on monoclonal antibody injections introduces new rules for biosimilars. The EMA now requires patient training materials to be part of equivalence assessments for inhalers-because if a patient doesn’t inhale correctly, the drug won’t work, regardless of the device.
Companies are turning to new tools. Physiologically-based pharmacokinetic (PBPK) modeling is now in 65% of complex generic submissions, up from 22% in 2018. These computer simulations predict how a drug will behave in the body based on its physical properties-cutting down the need for endless human trials.
Some are working with specialized CROs like Alimentiv or PRA Health Sciences, which have the equipment and expertise to run these studies. The FDA’s Complex Generic Drug Product Development program has helped 42 small businesses since 2018, offering free consultations and technical advice.
What’s Next? The Risks and the Future
There’s a quiet danger called “biocreep.” Imagine five generations of generic inhalers, each slightly different. Individually, each meets bioequivalence standards. But cumulatively, the particle size, plume shape, or release rate drifts. Over time, the final version might not work as well as the original. No one’s tracked this yet-but regulators are watching.
Still, the future is promising. With blockbuster drugs like Humira and Stelara losing patent protection, the demand for complex generics will surge. The market is projected to grow from $78 billion in 2022 to $112 billion by 2027.
And the goal remains clear: give patients access to affordable versions of life-changing drugs without compromising safety. That’s why bioequivalence for inhalers, patches, and injections isn’t just science-it’s a promise.
Why can’t we just use blood tests for inhalers and patches like we do for pills?
Because the drug isn’t meant to enter your bloodstream in the same way. For inhalers, the goal is local delivery to the lungs-so measuring blood levels doesn’t tell you if the drug reached the right place. For patches, the drug is released slowly over time, so peak blood levels (Cmax) aren’t meaningful. You need to test where the drug goes and how it’s released-not just how much shows up in your blood.
What happens if a generic inhaler passes blood tests but fails particle size tests?
It gets rejected. The FDA doesn’t approve products based on blood tests alone for inhalers. Particle size, plume shape, and dose uniformity are non-negotiable. One generic was turned down because 9% more drug stuck to the mouthpiece than the brand-even though blood levels were identical. The drug didn’t reach the lungs properly, so it wasn’t equivalent.
Are generic patches as effective as brand-name ones?
Yes-if they’re approved. Generic transdermal patches that meet FDA requirements for release rate, skin adhesion, and residual drug content perform just as well. Market data shows 65% penetration within three years of patent expiry. But if the patch doesn’t stick well or releases drug too fast, it fails. That’s why only about half of submitted patches get approved.
Why are complex injectables so hard to copy?
Because they’re not just drugs-they’re engineered systems. Liposomes, nanoparticles, and micelles have specific sizes, charges, and structures that affect how the body handles them. A 10% change in particle size can change how long the drug stays in circulation or where it accumulates. That’s why regulators demand exact matches in physical properties, not just drug concentration.
Is there a risk that multiple generic versions could make the drug less effective over time?
There’s a concern called “biocreep”-where small, approved differences across multiple generic versions add up over time. One version might have slightly smaller particles, the next a bit slower release. Individually, each meets standards. Together, they could drift from the original’s performance. Regulators are aware and are studying this, but no proven cases exist yet.
What Patients Should Know
If your doctor switches you to a generic inhaler or patch, don’t panic. If it’s approved by the FDA or EMA, it’s been tested under strict rules. But if you notice changes-like needing more puffs, the patch falling off, or side effects appearing-talk to your pharmacist. These systems are precise. Small differences matter.
The system isn’t perfect. It’s expensive, slow, and tough. But it’s designed to keep you safe. And for patients relying on these drugs every day, that’s worth every test, every instrument, every failed attempt.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.