Why Pediatric Medication Errors Are So Dangerous
Children aren’t just small adults. Their bodies process medicine differently, and even a tiny mistake in dosage can lead to serious harm-or death. One of the most common causes? Weight-based dosing errors. When a child needs a liquid antibiotic or painkiller, the dose isn’t just ‘a teaspoon.’ It’s calculated in milligrams per kilogram of body weight. Get the weight wrong, and you get the dose wrong. And it happens more than you think.
According to the World Health Organization, kids are three times more likely to suffer a medication error than adults. In the U.S., nearly 1 in 5 pediatric dosing mistakes comes from messing up the weight conversion-like confusing pounds and kilograms. A 2021 review of 63 studies found that over 32% of pediatric dispensing errors involved incorrect weight-based calculations. And 8.4% of those caused real harm: seizures, breathing problems, liver damage. These aren’t theoretical risks. They’re happening in hospitals, clinics, and even community pharmacies.
How Weight-Based Verification Works
Weight-based verification isn’t just a good idea-it’s now a standard. The American Society of Health-System Pharmacists (ASHP) says every pediatric facility must use it. The system isn’t magic. It’s a chain of checks built into how medicine is ordered, dispensed, and given.
Here’s how it works in practice:
- Weight is measured in kilograms only. No pounds. No ounces. Digital scales in pediatric units show weight to 0.1 kg for babies and 0.5 kg for older kids. If a scale shows pounds, it’s outdated.
- EHR systems block prescriptions without weight. If a doctor tries to order amoxicillin for a 3-year-old but hasn’t entered the weight, the system won’t let them submit it. The order is stuck until the weight is there.
- Pharmacists verify the math. The computer calculates the dose based on weight, but a pharmacist still reviews it. No automation replaces human judgment here.
- Barcode scanning at the bedside confirms weight and dose. When a nurse gives the medicine, they scan the child’s wristband, the medication, and the dose. If the weight doesn’t match the label, the system flags it.
This isn’t optional. It’s layered. One check fails? The next one catches it. That’s the point.
The Tech That Makes It Possible
None of this works without the right technology. The backbone is the Electronic Health Record (EHR) with built-in Clinical Decision Support Systems (CDSS). These aren’t just fancy forms-they’re smart rules programmed into the system.
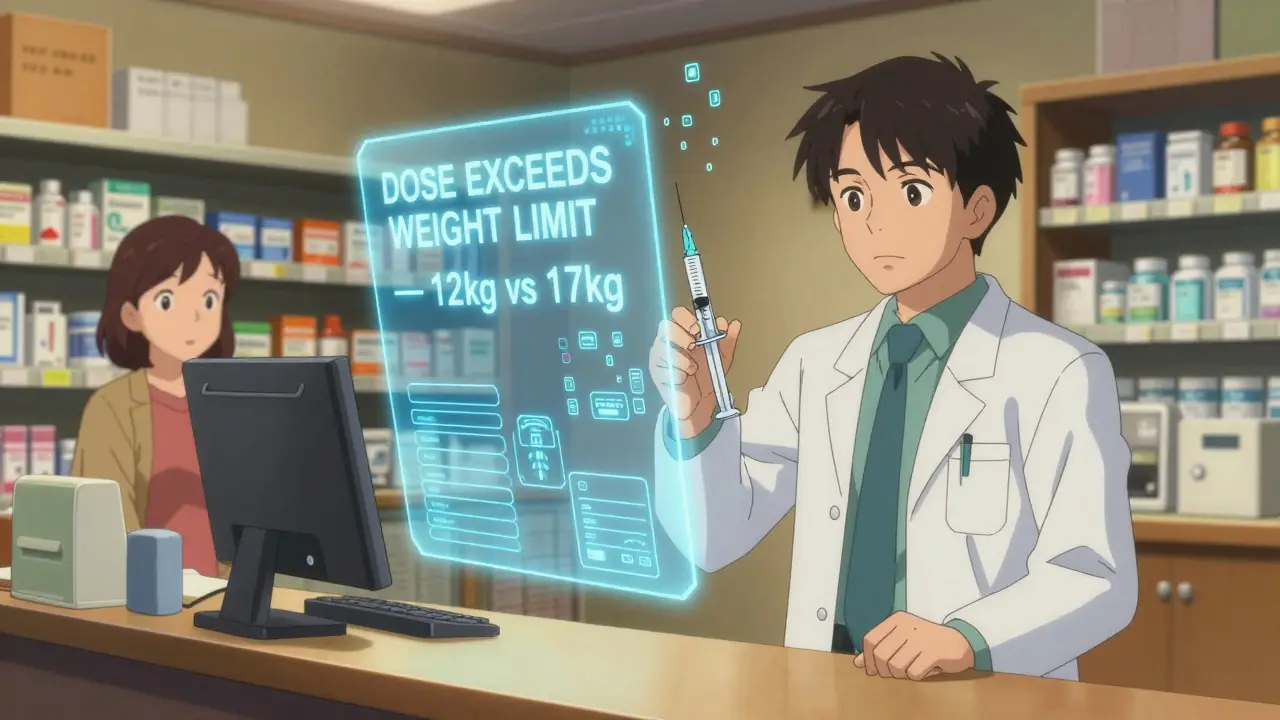
For example, if a child weighs 12 kg and the system knows that the safe upper limit for acetaminophen is 15 mg/kg per dose, it won’t allow a 250 mg dose. That’s too high. It’ll pop up a warning: “Dose exceeds recommended limit for weight.”
Studies show these systems cut dosing errors by up to 87% when set up right. But here’s the catch: they have to be customized. A hospital in Boston uses different dosing limits than one in rural Texas. The system must reflect local guidelines, drug concentrations, and patient populations.
Automated dispensing cabinets (ADCs) also help. These are the drug robots in the pharmacy that lock up medications. Modern ones pull the child’s weight from the EHR and only release the correct dose. If the weight is missing or outdated, the cabinet won’t open.
And barcode medication administration (BCMA)? That’s the scanner nurses use at the bedside. When weight data is linked to the barcode, the system knows if the dose being given matches the child’s current weight. One study found this cut administration errors by 74%.
Where It Falls Apart
Technology helps-but it doesn’t fix everything. The biggest problem? Outdated weights.
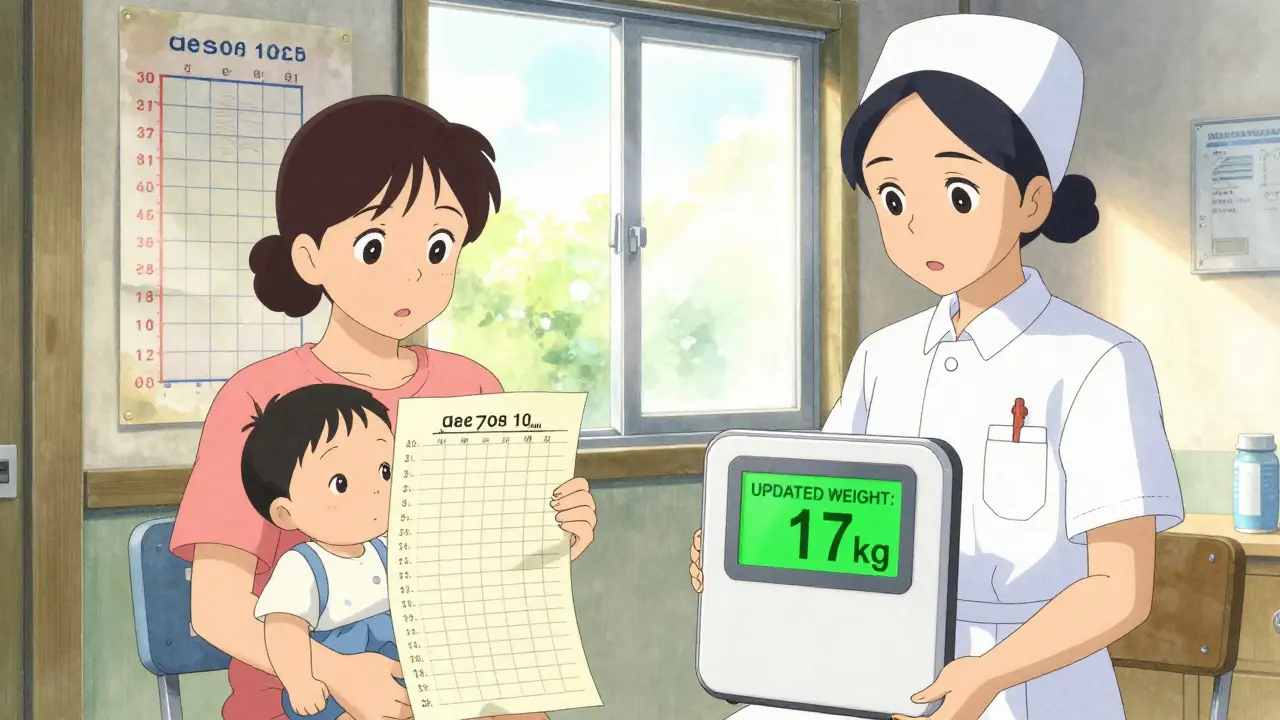
Imagine a child comes in for an ear infection. Their weight was last measured six months ago during a well-child visit. They’ve grown. The system still uses the old number. The pharmacist calculates the dose based on 14 kg, but the child now weighs 17 kg. The dose is too low. The infection doesn’t clear. The kid comes back. The error was silent. No one noticed.
The Institute for Safe Medication Practices (ISMP) says weights must be verified within 24 hours for acute care and every 30 days for outpatients. But in busy clinics, that’s hard. Nurses are overloaded. Parents forget to update weights. Electronic records don’t always sync between pediatricians and hospitals.
Another issue? Alert fatigue. EHRs can throw up so many warnings that clinicians start ignoring them. A 2021 study found that 41.7% of weight-based alerts were overridden. And of those overrides, 18.3% were actual errors that should’ve been caught. People got tired of clicking “Yes, I know this is wrong” and just moved on.
Community pharmacies are especially vulnerable. Most don’t have access to the child’s EHR. A parent walks in with a prescription. The pharmacist doesn’t know the child’s weight. They ask the parent. The parent guesses. “About 30 pounds?” That’s 13.6 kg-but they said 15. The dose is off. This happens more often than you’d think. One survey found nearly 30% of community pharmacists had a near-miss due to missing weight data every month.
What Actually Works: Real-World Fixes
Some places have cracked the code. Boston Children’s Hospital switched to kilogram-only scales, made weight entry mandatory in their EHR, and added pharmacist verification at every step. Over 18 months, weight conversion errors dropped from 14.3 per 10,000 doses to just 0.8. That’s a 94% reduction.
But it wasn’t easy. Pharmacists spent 37% more time verifying doses at first. Staff resisted. Training took 40 hours per person. They had to retrain doctors, nurses, pharmacists, and even the front desk staff who weigh kids on check-in.
Another win? Standardizing drug concentrations. Instead of having vancomycin come in 5 mg/mL, 10 mg/mL, and 20 mg/mL, they picked one standard. Fewer calculations. Fewer mistakes. One study showed this cut calculation errors by 72%.
And now, new tools are emerging. Epic Systems rolled out a new module in early 2024 that doesn’t just use weight-it uses growth charts. If a 5-year-old weighs 18 kg but is in the 98th percentile, the system knows they’re big for their age. It adjusts the safe dose range accordingly. In testing, it cut false alerts by 63%.
AI is starting to help too. ISMP is testing a system that predicts a child’s weight based on age, height, and past measurements. If the current weight doesn’t match the prediction, it flags it. Early results show 92% accuracy.
What You Can Do-Whether You’re a Parent, Nurse, or Pharmacist
You don’t need to be a doctor to help prevent these errors. Here’s what anyone can do:
- Parents: Always know your child’s current weight. Keep it written down. Bring it to every appointment. Say: “My child weighs 22 kg.” Don’t wait to be asked.
- Nurses: Weigh every child on admission. Even if they were weighed last week. Update the chart. If the weight looks off, question it.
- Pharmacists: Never dispense a pediatric dose without verifying the weight. If the EHR doesn’t have it, call the prescriber. Don’t guess. Don’t assume.
- Doctors: Don’t skip the weight field. If your EHR lets you order without it, don’t. Make it mandatory in your practice.
And if you’re in a clinic or hospital without a full system? Start small. Get digital scales. Train staff on kilogram-only use. Make weight a required field in every pediatric order. It doesn’t take a million-dollar system to save a life. Just a little discipline.
The Bigger Picture
Weight-based verification isn’t just a technical fix. It’s a cultural one. It means accepting that mistakes happen-and building systems to catch them before they hurt someone. The Leapfrog Group now requires it for hospitals to get an “A” safety rating. Medicare and Medicaid now demand it for reimbursement. The market for pediatric safety tech is set to hit $2.3 billion by 2027.
But the gap remains. In big children’s hospitals, 94% have full systems. In rural clinics? Only 33%. That means kids in small towns are still at higher risk. That’s not fair. And it’s not safe.
Technology will keep improving. AI, wearables, blockchain-maybe one day, a child’s weight will update automatically from a smart scale at home. But until then, the simplest things work best: accurate numbers, clear communication, and people who refuse to let a mistake slide.
One wrong dose can change a family’s life forever. Getting the weight right? That’s the first, and most important, step.


Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.