When it comes to managing Myasthenia Gravis, Mestinon is often the first name that pops up. Mestinon (pyridostigmine) is an acetylcholinesterase inhibitor that boosts nerve‑muscle communication, easing muscle weakness. But it isn’t the only option on the table. In this guide we’ll line up Mestinon against the most common alternatives, break down how they work, compare dosing and side‑effect profiles, and point out the situations where one might be a better fit than the other.
Why a Comparison Matters
- Patients often wonder if switching drugs could reduce fatigue.
- Doctors need clear data to tailor therapy for fluctuating symptoms.
- Insurance formularies sometimes favor one medication over another.
Having a side‑by‑side view helps you make an evidence‑based choice, whether you’re in a clinic or reviewing your own prescription.
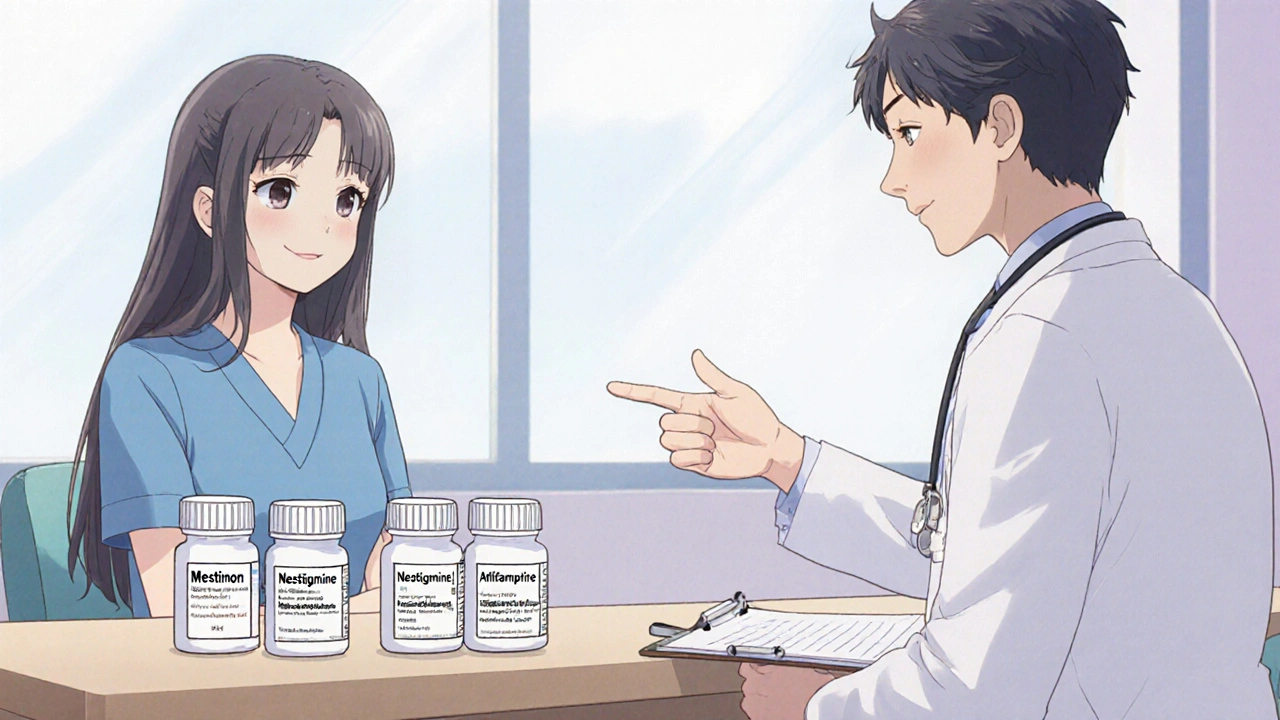
Core Players in the Market
Below are the drugs that most clinicians consider when prescribing for Myasthenia Gravis:
- Mestinon (Pyridostigmine) - the classic oral anticholinesterase.
- Neostigmine - a shorter‑acting injectable alternative.
- Amifampridine (Firdapse) - a newer potassium channel blocker approved for Lambert‑Eaton myasthenic syndrome and off‑label for Myasthenia.
How Each Drug Works
All three agents aim to improve neuromuscular transmission, but they take different routes:
- Acetylcholinesterase inhibition - Both Mestinon and Neostigmine block the enzyme that breaks down acetylcholine, letting more of the neurotransmitter stay available at the neuromuscular junction.
- Potassium channel blockade - Amifampridine prolongs the action potential in presynaptic nerves, boosting acetylcholine release.
Understanding the mechanism clarifies why side‑effects differ. For example, anticholinesterases can cause excessive sweating, whereas potassium channel blockers often lead to paresthesia.
Typical Dosing Regimens
| Drug | Formulation | Starting Dose | Typical Maintenance Range |
|---|---|---|---|
| Mestinon | Oral tablet | 30 mg 3‑times daily | 60‑180 mg per day, divided 3‑4 doses |
| Neostigmine | Intravenous or subcutaneous injection | 0.5‑1 mg every 30‑60 min (hospital setting) | 0.5‑2 mg/hour continuous infusion for severe cases |
| Amifampridine | Oral capsule | 5 mg twice daily | 10‑30 mg daily, split into 2‑3 doses |
Note that dosing is highly individualized. Blood levels, symptom severity, and renal function all influence the final numbers.
Side‑Effect Profiles
Side effects often dictate whether a patient can stay on a particular drug long term.
| Drug | Most Frequent | Less Common but Serious |
|---|---|---|
| Mestinon | Diarrhea, abdominal cramps, increased salivation | Bradycardia, severe bronchospasm |
| Neostigmine | Muscle fasciculations, sweating, nausea | Cholinergic crisis (muscle weakness worsening) |
| Amifampridine | Paresthesia, nausea, headache | Seizures (rare), cardiac arrhythmias |
Patients with pre‑existing gastrointestinal issues often prefer Amifampridine, while those with cardiac concerns may avoid high‑dose anticholinesterases.
Drug Interactions to Watch
Because these agents affect neurotransmitter pathways, they can clash with other meds:
- Beta‑blockers - May worsen bradycardia when combined with Mestinon.
- Anticholinergic drugs (e.g., diphenhydramine) - Counteract the therapeutic effect of anticholinesterases.
- Other potassium channel blockers - Can increase the risk of arrhythmias with Amifampridine.
Always review the full medication list with your neurologist before adding or switching drugs.
Clinical Evidence and FDA Status
Regulatory approval and trial data give confidence in choosing a therapy:
- Mestinon - FDA‑approved for Myasthenia Gravis since the 1950s; backed by decades of real‑world data.
- Neostigmine - Approved for myasthenic crisis and postoperative residual curarization; often used off‑label for chronic control.
- Amifampridine - Gained FDA approval for Lambert‑Eaton in 2018; 2022 studies showed benefit in refractory Myasthenia Gravis, leading many clinicians to consider it off‑label.
When insurance asks for “step‑therapy,” Mestiton’s long‑standing approval usually meets the requirement first.
How to Choose the Right Option
Pick the drug that aligns with three practical pillars:
- Symptom pattern - Rapidly fluctuating weakness may respond better to short‑acting Neostigmine in a hospital setting.
- Side‑effect tolerance - If diarrhea is a deal‑breaker, consider Amifampridine.
- Accessibility and cost - Mestinon is widely available as a generic; Amifampridine can be pricey and may need prior authorization.
Discuss these factors with your neurologist, and don’t hesitate to ask for a trial period to see how you feel.
Quick Takeaways
- Mestinon remains the first‑line oral therapy for most Myasthenia Gravis patients.
- Neostigmine offers rapid, injectable control but requires careful monitoring.
- Amifampridine is a newer, non‑anticholinesterase option useful when traditional drugs cause intolerable side effects.
- Side‑effect profiles and drug interactions differ enough to influence long‑term adherence.
- Cost and insurance coverage often tip the scale toward Mestinon unless a specific clinical need calls for alternatives.
Can I take Mestinon and Amifampridine together?
Combining two agents that enhance acetylcholine can raise the risk of cholinergic overload. Most specialists recommend using one drug at a time and only switching under close supervision.
What should I do if I experience severe diarrhea on Mestinon?
Contact your neurologist right away. The dose can be lowered, or you might switch to an alternative like Amifampridine that has a milder gastrointestinal profile.
Is Neostigmine only for hospital use?
Because Neostigmine works quickly and can cause rapid changes in muscle strength, it’s usually reserved for acute settings or crisis management. Some patients use a home‑infusion pump, but that requires strict monitoring.
How does insurance typically handle Amifampridine?
Amifampridine is often classified as a specialty drug with higher copays. Expect a prior‑authorization request and be prepared to provide documentation of intolerance or inadequate response to anticholinesterases.
Are there lifestyle changes that can boost medication effectiveness?
Yes. Maintaining a stable sleep schedule, avoiding extreme temperatures, and managing stress can reduce symptom swings, letting any of the drugs work more predictably.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.