When a child needs medicine, getting the dose right isn't just important-it's life-or-death. A mistake of even a few milligrams can turn a helpful treatment into a dangerous overdose. That's why weight-based dosing is the gold standard in pediatric care. It’s not a suggestion. It’s a safety rule built on decades of evidence, and it’s backed by hospitals, regulators, and frontline nurses alike.
Why Weight Matters More Than Age
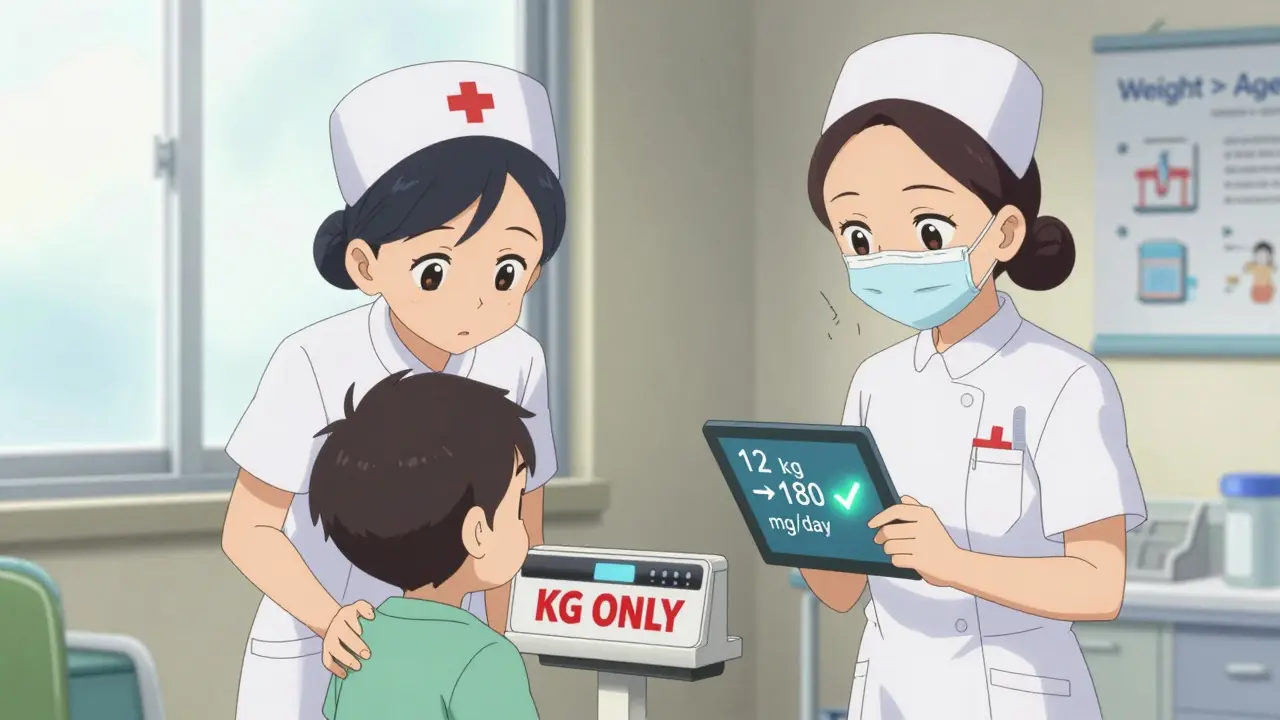
Many people assume that a child’s age tells you how much medicine they need. But that’s risky. A 2-year-old weighing 10 kg and another weighing 18 kg may be the same age, but their bodies process drugs completely differently. Kids aren’t just small adults. Their bodies have more water, less fat, and organs that aren’t fully developed-especially in babies under 6 months. Their kidneys and liver can’t clear drugs the way an adult’s can. That’s why using age alone leads to errors in nearly one-third of cases, according to the Journal of Clinical Pharmacy and Therapeutics. Weight-based dosing cuts through that guesswork. Instead of asking, “How old are you?” providers ask, “How much do you weigh?” Then they calculate the dose using milligrams per kilogram (mg/kg). This method is used in 87% of hospital settings for children, as reported by Davis’s Drug Guide (2023). For example, if a child is prescribed 15 mg/kg of amoxicillin and weighs 12 kg, the total daily dose is 180 mg. If it’s given twice a day, each dose is 90 mg. Simple. Precise. Repeatable.The Three Steps to Get It Right
Getting the math right takes more than just plugging numbers into a calculator. There’s a process-and skipping steps causes most errors. Here’s how it works:- Convert pounds to kilograms. If the scale says 44 pounds, divide by 2.2. That’s 20 kg. Never round until the final answer. Rounding too early can throw off the whole calculation.
- Multiply weight by the prescribed dose. If the order is 20 mg/kg/day and the child weighs 20 kg, the total daily dose is 400 mg.
- Divide by frequency. If it’s given twice daily, each dose is 200 mg.
The Double-Check That Saves Lives
Even the best calculations can go wrong. A nurse might misread the scale. A doctor might type 5 mg/kg instead of 0.5 mg/kg. That’s why every major children’s hospital requires a second person to verify every weight-based dose-especially for high-risk medications like insulin, opioids, or chemotherapy. The Joint Commission’s National Patient Safety Goal 01.01.01 says: “Independent double-checks are mandatory for high-alert medications.” This isn’t a formality. It’s a safety net. In a 2022 meta-analysis of 87,342 pediatric doses, the American College of Clinical Pharmacy found that double-checking reduced serious errors by 68%. That’s two out of every three dangerous mistakes prevented. One pediatric nurse in Perth shared how her hospital changed its practice after a near-miss. “We had a scale that defaulted to pounds,” she said. “One day, a 5 kg baby was weighed at 11 pounds. Someone thought that meant 11 kg. The dose was way too high. We now have bright red stickers on every scale: ‘WEIGH IN KG ONLY.’”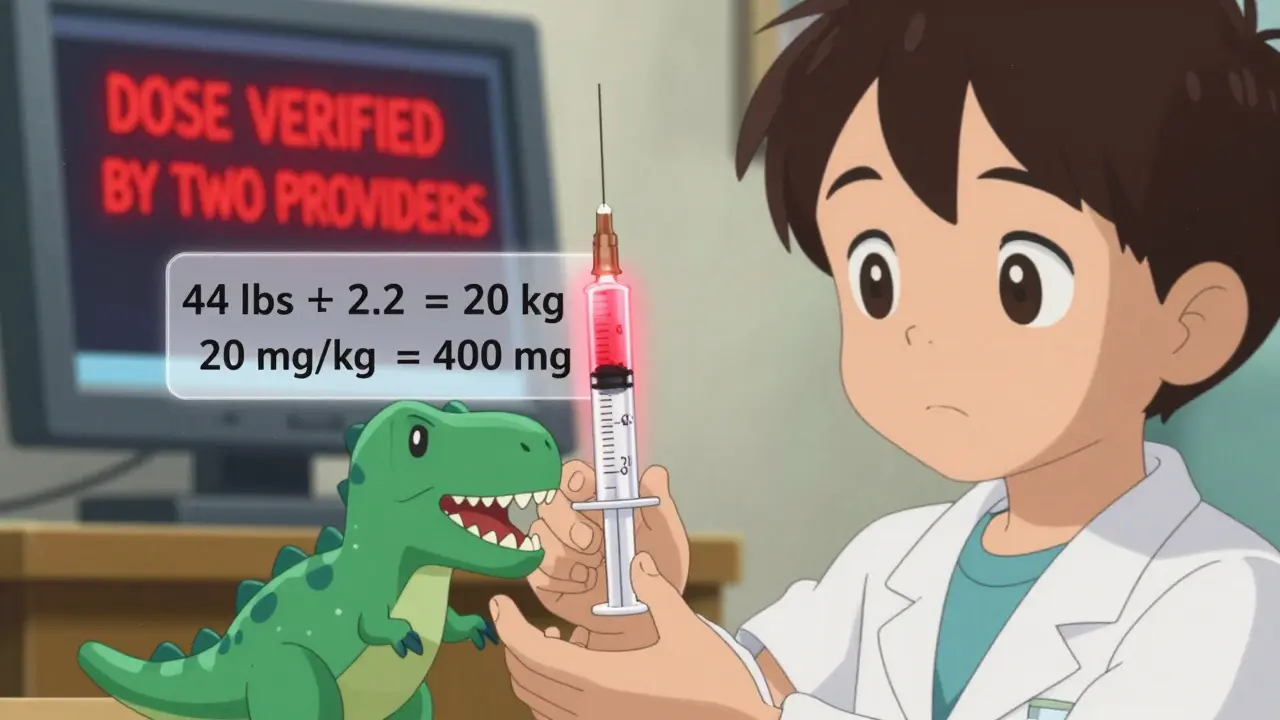
Where Things Go Wrong
Despite the clear guidelines, errors still happen. The Institute for Safe Medication Practices (ISMP) tracked 1,247 pediatric dosing errors in 2022. The top three causes:- Unit conversion mistakes (38%): Mixing up pounds and kilograms. This is still the #1 error, even in 2026.
- Decimal point slips (27%): Typing 5.0 mg instead of 0.5 mg. It’s easy to miss a zero.
- Ignoring organ function (19%): Giving a full dose to a premature infant with immature kidneys. Weight doesn’t tell the whole story.
Special Cases: Obesity and BSA
Not every child is average. Kids with obesity need special attention. A child with a BMI over the 95th percentile might weigh 50 kg, but their body composition is mostly fat-not muscle or water. For drugs that dissolve in water (like antibiotics), using their full weight can lead to overdose. For drugs that dissolve in fat (like some seizure meds), underdosing is the risk. The Pediatric Endocrine Society recommends using adjusted body weight for these cases: Adjusted Weight = Ideal Weight + 0.4 × (Actual Weight − Ideal Weight). This formula balances safety and effectiveness. About 78% of children’s hospitals now use it, according to the Children’s Hospital Association. Body Surface Area (BSA), calculated using height and weight, is more accurate for chemotherapy drugs. The Mosteller formula: √(weight in kg × height in cm ÷ 3600). But it takes longer. A 2023 University of Michigan study found BSA calculations added 47 seconds per dose. That’s why it’s used only for specific drugs-not routine prescriptions.Technology Is Helping-But Not Replacing
Electronic health records (EHRs) now have built-in pediatric dosing tools. Epic Systems rolled out pediatric modules in June 2023 that auto-calculate doses, flag out-of-range amounts, and block unsafe orders. These systems are now in 78% of children’s hospitals. They’ve cut dosing errors by over 50% in places like UCSF Medical Center. But technology isn’t perfect. One nurse told me: “I saw an EHR suggest 100 mg of morphine for a 3-year-old. The system didn’t know the child had kidney failure. The nurse caught it because she knew the history.” Algorithms can’t replace clinical judgment. They just make it easier to spot mistakes.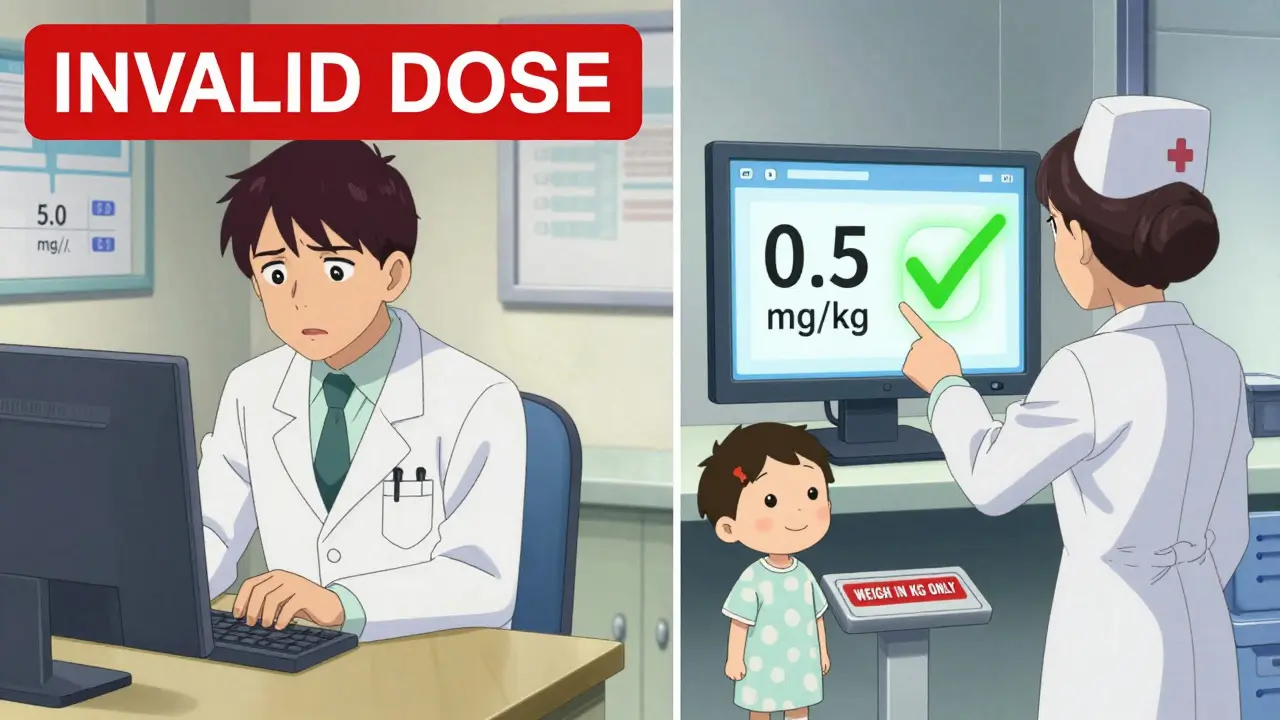
What You Need to Remember
- Always use kilograms. No exceptions. If the scale is in pounds, convert it. Don’t assume. - Never round until the final number. Round too early, and your dose is wrong. - Double-check every high-alert drug. Two qualified people must verify the weight, the math, and the final dose. - Know the limits. Every drug has a maximum safe dose. If the calculated dose exceeds it, stop and recheck. - Consider development, not just weight. A 3-month-old and a 3-year-old with the same weight need different doses because their bodies work differently.Training and Compliance
The Pediatric Nursing Certification Board requires all pediatric nurses to pass a 25-question exam on dosing calculations with a 90% score-every year. Hospitals that skip this training see twice as many errors. It’s not optional. It’s mandatory. In Australia, the Therapeutic Goods Administration (TGA) now requires all drug labels to include pediatric weight-based dosing instructions. This change, implemented in 2024, means pharmacists can’t just rely on old charts anymore. They have to calculate based on weight-every time.Looking Ahead
The future of pediatric dosing is moving toward precision. The NIH’s Pediatric Trials Network has enrolled over 15,000 children to build better dosing rules for 25 common drugs. The FDA is requiring all new drugs to include pediatric algorithms by 2025. Genetic testing for drug metabolism (like CYP2D6) is starting to guide opioid dosing in teens. But no matter how advanced the tech gets, the foundation won’t change. Weight-based dosing, with a second set of eyes, remains the most reliable way to keep children safe. It’s not glamorous. It’s not flashy. But it’s the difference between a child getting better-and a child getting hurt.Why is weight-based dosing better than age-based dosing for children?
Weight-based dosing accounts for actual body size and physiology, while age-based dosing assumes all children of the same age have similar body composition. Research shows weight-based dosing reduces medication errors by 43% compared to age-based estimates. A 2-year-old weighing 8 kg and another weighing 18 kg may be the same age, but their drug metabolism, water content, and organ function differ greatly-making weight the only reliable predictor of safe dosing.
What is the most common mistake in pediatric weight-based dosing?
The most common mistake is confusing pounds and kilograms. A 2022 ISMP report found that 38% of pediatric dosing errors came from incorrect unit conversion. For example, a child weighing 22 pounds (10 kg) was mistakenly treated as 22 kg, leading to a 120% overdose. Hospitals now use red stickers on scales that say “WEIGH IN KG ONLY” to prevent this.
Do all children need a double-check before receiving medication?
No-not every child. But for high-alert medications like opioids, insulin, chemotherapy, and anticoagulants, a double-check is mandatory under The Joint Commission’s safety standards. Two qualified providers must independently verify the weight, the calculation, and the final dose. This practice reduces serious errors by 68%, according to a 2022 meta-analysis of over 87,000 doses.
How do you calculate weight in kilograms from pounds?
Divide the weight in pounds by 2.2. For example, a child weighing 33 pounds is 33 ÷ 2.2 = 15 kg. Never round the result until after you’ve completed the full calculation. Rounding too early can lead to cumulative errors. Always use the exact number for multiplication and division steps.
Is body surface area (BSA) better than weight-based dosing?
For most medications, weight-based dosing is simpler and just as accurate. But for chemotherapy drugs, BSA (calculated using height and weight) is more precise. A 2021 study found BSA dosing improved accuracy by 18% for cancer drugs. However, it takes longer-about 47 seconds more per dose-and requires knowing the child’s height. Most hospitals use BSA only for specific drugs, not routine prescriptions.

Graham Holborn
Hi, I'm Caspian Osterholm, a pharmaceutical expert with a passion for writing about medication and diseases. Through years of experience in the industry, I've developed a comprehensive understanding of various medications and their impact on health. I enjoy researching and sharing my knowledge with others, aiming to inform and educate people on the importance of pharmaceuticals in managing and treating different health conditions. My ultimate goal is to help people make informed decisions about their health and well-being.