Bioequivalence: What It Means for Generic Drugs and Your Health
When you pick up a generic pill, you want to know it will do the same job as the brand-name version. That’s where bioequivalence, the scientific standard that proves two drug formulations produce the same effect in the body. Also known as therapeutic equivalence, it’s the reason your pharmacist can legally swap a brand drug for a cheaper generic without risking your health. It’s not just about matching ingredients—it’s about proving your body absorbs and uses the medicine the exact same way. If a generic doesn’t meet this bar, it’s not approved.
The FDA, the U.S. agency that sets drug safety and effectiveness rules requires strict testing for bioequivalence before any generic hits the shelf. They don’t just look at the pill’s ingredients—they measure how fast and how much of the drug enters your bloodstream. This is done through blood tests in healthy volunteers, comparing the generic to the original brand. The results must fall within a narrow range: 80% to 125% of the brand’s absorption rate. If it’s outside that range, the generic gets rejected. This isn’t a formality—it’s a safety net. A drug that’s absorbed too quickly could cause side effects. One that’s absorbed too slowly might not work at all.
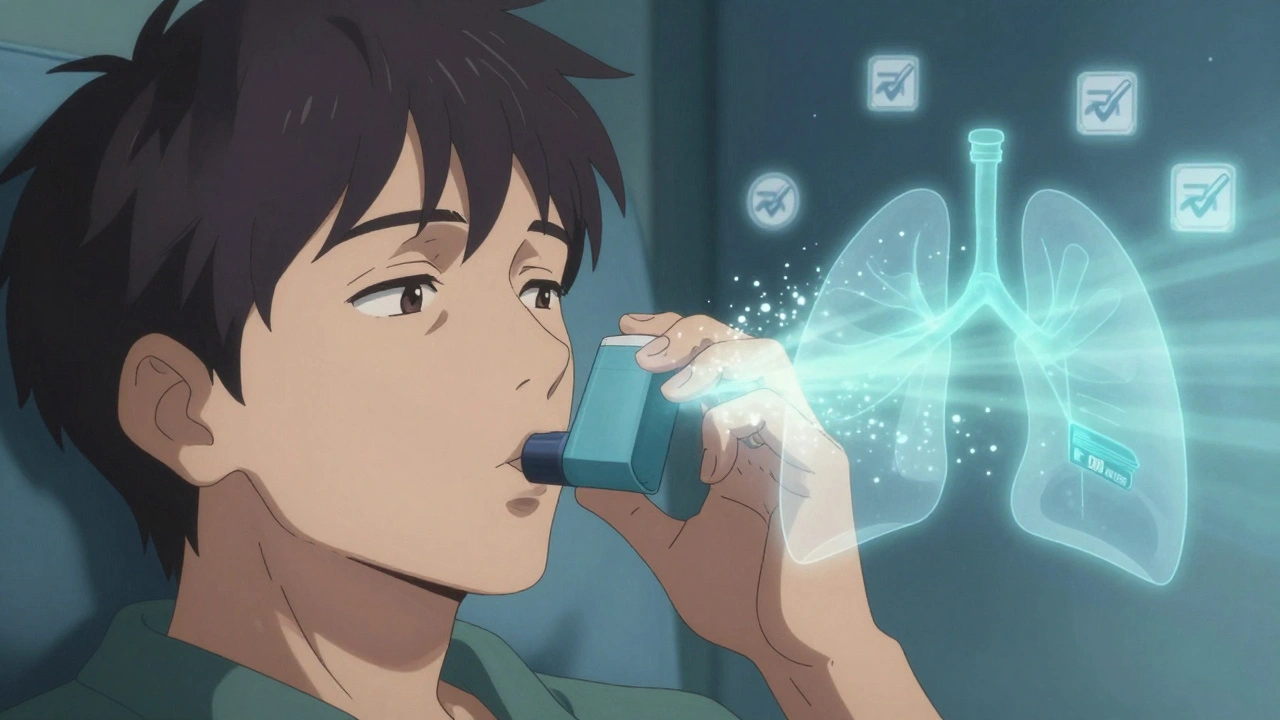
Bioequivalence isn’t just about pills. It applies to creams, inhalers, injections, and even liquid forms. That’s why a generic asthma inhaler or a topical steroid cream must prove it delivers the same dose to the right place in your body. You’ll see this concept pop up in posts about authorized generics, brand-name drugs made by the same company but sold under a different label, because they’re identical by design. You’ll also see it in discussions about biosimilars, complex biologic drugs that can’t be exact copies but must still prove similar enough to work the same way. Even when a drug has a black box warning or interacts with grapefruit, bioequivalence ensures the generic version carries the same risks and benefits as the original.
What this means for you is simple: if a generic is FDA-approved, you can trust it. No need to worry you’re getting a weaker version. The science behind bioequivalence is rigorous, and the data is public. It’s why millions of people switch to generics every year—because they save money without sacrificing results. But it’s also why you should never swap between different generic brands without checking with your doctor or pharmacist. Even if both are bioequivalent to the brand, two different generics might not be bioequivalent to each other. That’s why consistency matters.
Below, you’ll find real-world examples of how bioequivalence plays out in daily medication use—from heart pills and antibiotics to hormone treatments and cholesterol drugs. You’ll see how it connects to drug safety, cost savings, and what to ask your pharmacist when you’re handed a new bottle. This isn’t theory. It’s the quiet rule that keeps your prescriptions working, no matter the price tag.