Combination Cholesterol Therapy: What Works, What Doesn’t, and What to Watch For
When combination cholesterol therapy, using two or more drugs together to lower LDL cholesterol when one drug isn’t enough. Also known as dual lipid-lowering therapy, it’s a common next step for people who still have high cholesterol despite taking a statin. It’s not just about adding more pills—it’s about picking the right mix that works without risking side effects.
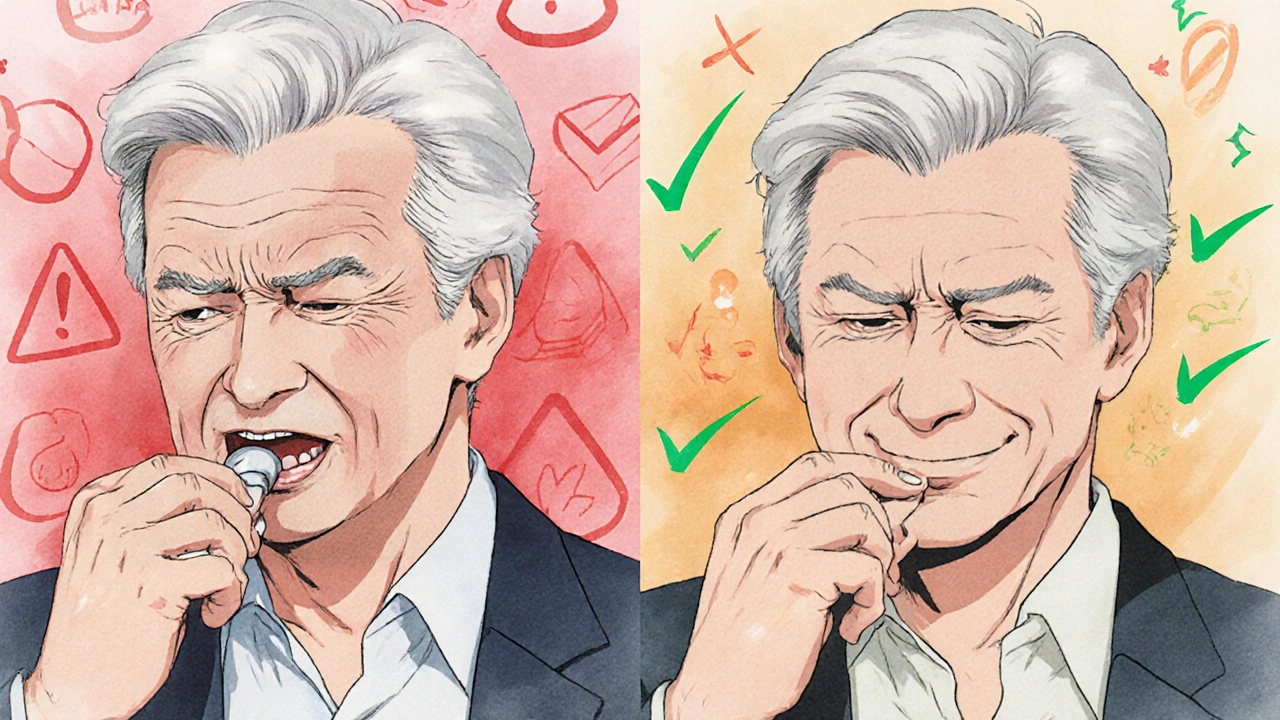
Most combination therapies start with a statin, a class of drugs that block cholesterol production in the liver and add a second agent like ezetimibe, a drug that reduces cholesterol absorption in the gut. This combo is safe, well-studied, and often covered by insurance. For tougher cases, doctors may add a PCSK9 inhibitor, a powerful injectable that helps the liver pull more LDL out of the blood. These are newer, more expensive, and usually reserved for high-risk patients. But here’s the catch: not all combinations are equal. Grapefruit can mess with some statins, and mixing certain drugs can raise the risk of muscle damage or liver stress. You can’t just stack pills and hope for the best.
What you’ll find in this collection isn’t just a list of drug names. It’s real-world guidance on what combinations actually work, what interactions to avoid, and how to spot the warning signs when something’s off. You’ll see how grapefruit affects statins, why authorized generics matter when you’re on long-term therapy, and how drug safety programs like REMS impact your access to high-risk combos. There’s no fluff—just clear, practical info from people who’ve been through it. Whether you’re just starting combination therapy or have been on it for years, these posts help you ask the right questions and stay in control.