Drug Noncompliance: Why People Skip Medications and What It Costs
When someone stops taking their medicine even though it was prescribed, that’s drug noncompliance, the failure to follow a prescribed medication plan, whether by skipping doses, stopping early, or not filling prescriptions. Also known as medication nonadherence, it’s not laziness—it’s often confusion, cost, fear, or side effects that push people away from their treatment. This isn’t a small issue. The CDC says nearly half of Americans don’t take their meds as directed. And it’s not just about missing pills—it’s about broken outcomes: more ER visits, worse disease control, and avoidable deaths.
Why does this happen? For some, it’s the price. A single pill costing $100 a month means choosing between medicine and groceries. For others, it’s complexity. Taking five different pills at different times with food or on an empty stomach? That’s a recipe for forgetting. And then there’s fear. If you’ve read a prescription drug label and seen a black box warning about liver damage or serotonin syndrome, it’s natural to pause. That’s why drug interactions, when two or more medications interfere dangerously, like SSRIs with opioids or rifampin with birth control matter so much. If you don’t understand why you’re taking a drug—or worse, if you’ve heard stories about it causing harm—you’re more likely to quit.
And it’s not just about the patient. The system plays a role too. If your doctor prescribes a combination cholesterol therapy, a single pill that combines statins with ezetimibe to lower LDL but you can’t afford it, or if you’re handed a bottle of generic pills with no explanation, compliance drops fast. Even the packaging matters. If you’re buying counterfeit drugs, fake pills with no active ingredient or toxic fillers because you can’t afford the real thing, you’re not being noncompliant—you’re being forced into a dangerous workaround.
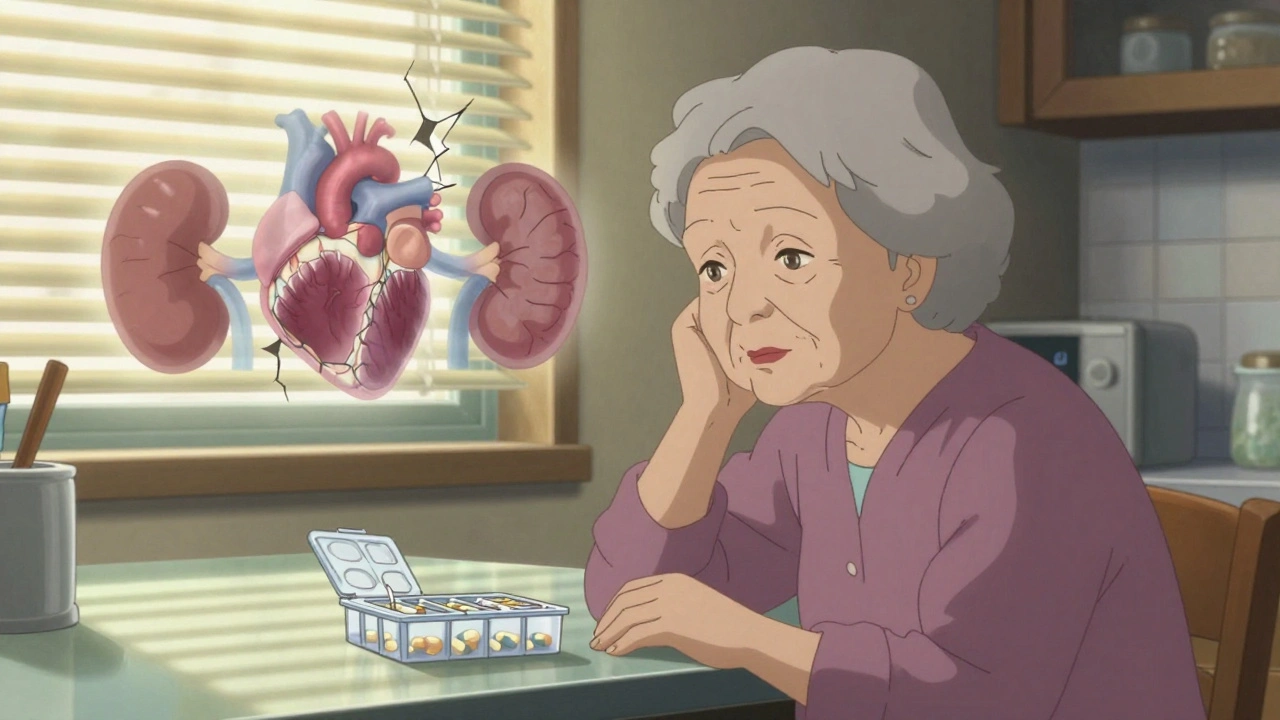
Drug noncompliance doesn’t happen in a vacuum. It’s tied to how we deliver care, how we label warnings, how we price medicines, and whether patients feel heard. That’s why the posts here cover everything from how to read a prescription drug label to why geriatric medication safety, the careful management of drugs in older adults to avoid dangerous side effects and polypharmacy needs special attention. You’ll find guides on how REMS programs, FDA safety plans that require special training for doctors and pharmacies to manage high-risk drugs try—and sometimes fail—to keep people safe. You’ll see how bioequivalence, the standard that ensures generics work just like brand-name drugs gives people cheaper options, but doesn’t always fix trust issues.
What you’ll find below isn’t just a list of articles. It’s a map of the real-world reasons people stop taking their meds—and what can be done about it. Whether you’re a patient, a caregiver, or just trying to understand why so many prescriptions go unused, these posts give you the facts without the fluff. No jargon. No sugarcoating. Just what works, what doesn’t, and why it matters.