Grapefruit Drug Interaction: What You Need to Know Before Taking Medication
When you eat grapefruit, a citrus fruit known for its tart flavor and high vitamin C content. Also known as pomelo hybrid, it can interfere with how your body processes many common medications. This isn’t just a minor warning—it’s a serious risk that can lead to overdose, organ damage, or even death. The problem isn’t the fruit itself, but how it changes the way your liver and intestines break down drugs. If you’re on any prescription meds, skipping grapefruit might save your life.
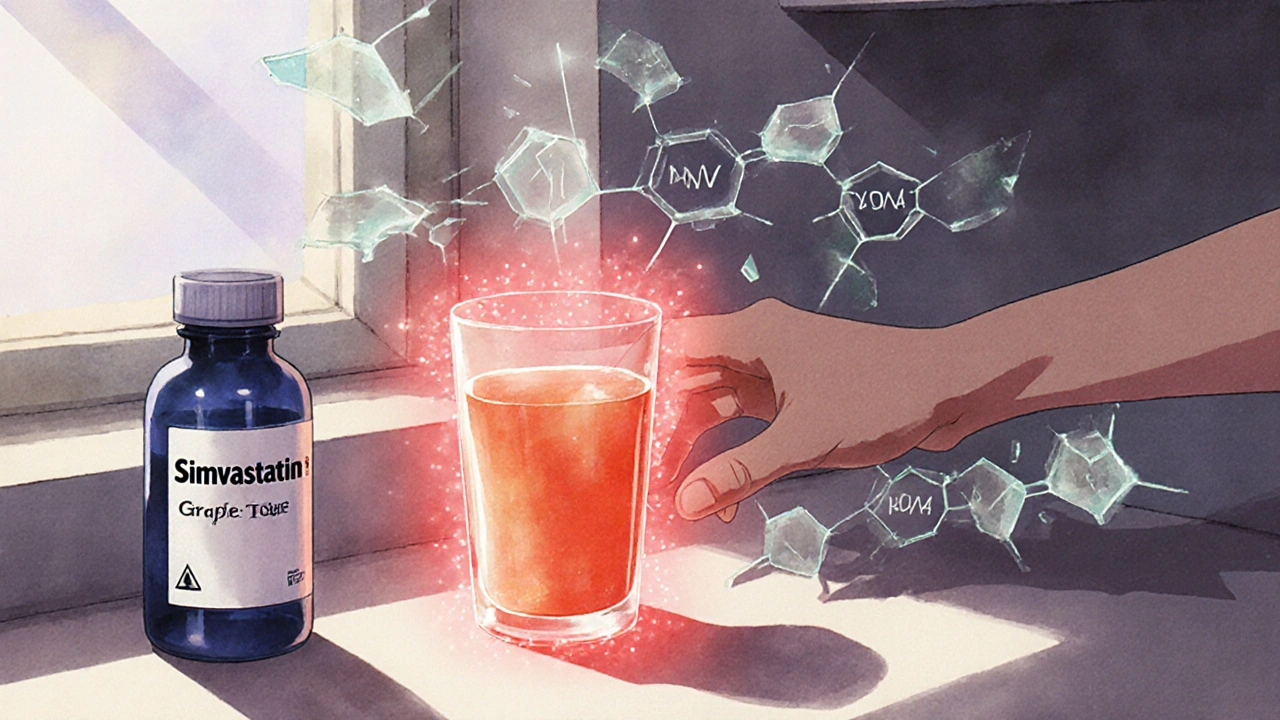
This grapefruit drug interaction happens because grapefruit blocks an enzyme called CYP3A4, which normally helps break down over 85 medications. When that enzyme is shut down, drugs build up in your bloodstream at levels far higher than intended. It doesn’t matter if you eat half a grapefruit, drink a glass of juice, or even take a single serving—once the enzyme is blocked, the effect lasts over 24 hours. This isn’t a myth or an old wives’ tale. The FDA has issued warnings on this for years, and studies show that even small amounts can spike blood levels of statins, blood pressure drugs, and immunosuppressants by 300% or more. The same goes for other citrus fruits like Seville oranges and pomelos, but not regular oranges or lemons.
Some of the most dangerous combinations include statins like simvastatin (Zocor), which can cause muscle breakdown; calcium channel blockers like amlodipine, which can crash your blood pressure; and immunosuppressants like cyclosporine, which can lead to kidney failure. Even common drugs like sildenafil (Viagra) or certain anti-anxiety meds can become risky. The scary part? You won’t feel anything until it’s too late. There’s no warning sign—no dizziness, no nausea, no immediate reaction. That’s why this interaction is so dangerous: it’s silent, invisible, and often overlooked by doctors and patients alike.
What makes this even trickier is that not all medications are affected the same way. Some drugs, like lisinopril or metformin, are completely safe with grapefruit. But unless you know exactly which ones are risky, the safest move is to avoid it entirely while on any new prescription. Always ask your pharmacist: "Does this interact with grapefruit?" Don’t assume it’s fine because your doctor didn’t mention it. Most don’t bring it up unless you ask. And if you’re taking multiple meds, the risk multiplies—especially with drugs already flagged for narrow therapeutic windows, like those used for heart rhythm or epilepsy.
Below, you’ll find real, practical guides from people who’ve been there—whether it’s understanding how grapefruit affects cholesterol meds, why some generics behave differently than brand names, or how to spot hidden risks in common prescriptions. These aren’t theoretical articles. They’re written by patients and clinicians who’ve seen the fallout firsthand. You’ll learn what to avoid, what’s safe, and how to talk to your doctor without sounding paranoid. This isn’t about fear. It’s about control. You deserve to take your meds safely—and that starts with knowing what’s in your fridge.