Opioid Overdose: Signs, Risks, and What to Do Now
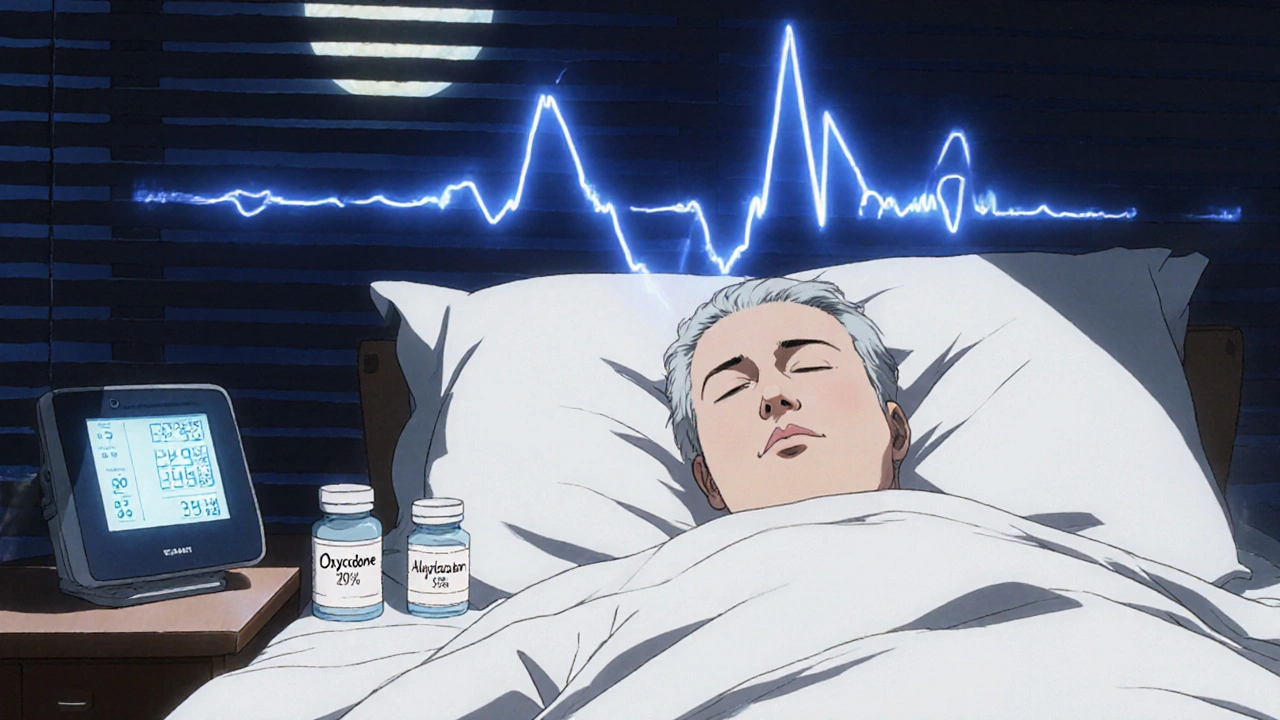
When someone experiences an opioid overdose, a life-threatening condition caused by too much opioid in the body, leading to stopped or slowed breathing. Also known as opioid poisoning, it’s one of the leading causes of preventable death in adults today. It doesn’t matter if the drug is prescription painkillers like oxycodone, illegal heroin, or synthetic fentanyl—even a small amount can shut down breathing. The body doesn’t need much to stop working, and time is the one thing you can’t afford to waste.
Naloxone, a medication that reverses opioid overdose by blocking opioid receptors in the brain. Also known as Narcan, it’s safe, easy to use, and works in minutes. You don’t need to be a doctor to give it. Emergency responders, family members, even strangers have saved lives by keeping naloxone on hand. But it’s not a cure—it’s a bridge. Someone who gets naloxone still needs urgent medical care. Without it, the overdose can return once the drug wears off.
The opioid crisis, a public health emergency fueled by overprescribing, addiction, and the rise of deadly synthetic opioids like fentanyl. It’s not just about street drugs. Many overdoses start with a prescription that turns into dependence. People don’t wake up one day wanting to use heroin—they start with pain pills after surgery, then lose control. The line between treatment and addiction is thin, and the risk of overdose grows with every extra pill.
Knowing the signs saves lives. Slowed or stopped breathing, blue lips or fingernails, unresponsiveness, gurgling sounds like choking—these aren’t signs of being drunk or asleep. They’re signs of an overdose. If you see them, act. Call 911. Give naloxone if you have it. Start chest compressions if the person isn’t breathing. Don’t wait for someone to "wake up on their own." They won’t.
This collection brings together real, practical guides on how opioids affect the body, how to spot trouble before it’s too late, and what tools and strategies actually work. You’ll find clear breakdowns of how naloxone works, why fentanyl is so dangerous, how to talk to someone struggling with addiction, and what pharmacies and clinics are doing to prevent overdoses. These aren’t theory pieces—they’re tools for real life.
If you’re reading this because you’re worried about someone—or because you’re worried about yourself—you’re not alone. And help is closer than you think. The posts below give you the facts, not fear. No fluff. No jargon. Just what you need to know to act, protect, and survive.