Opioids and Benzodiazepines: Risks, Interactions, and Safer Choices
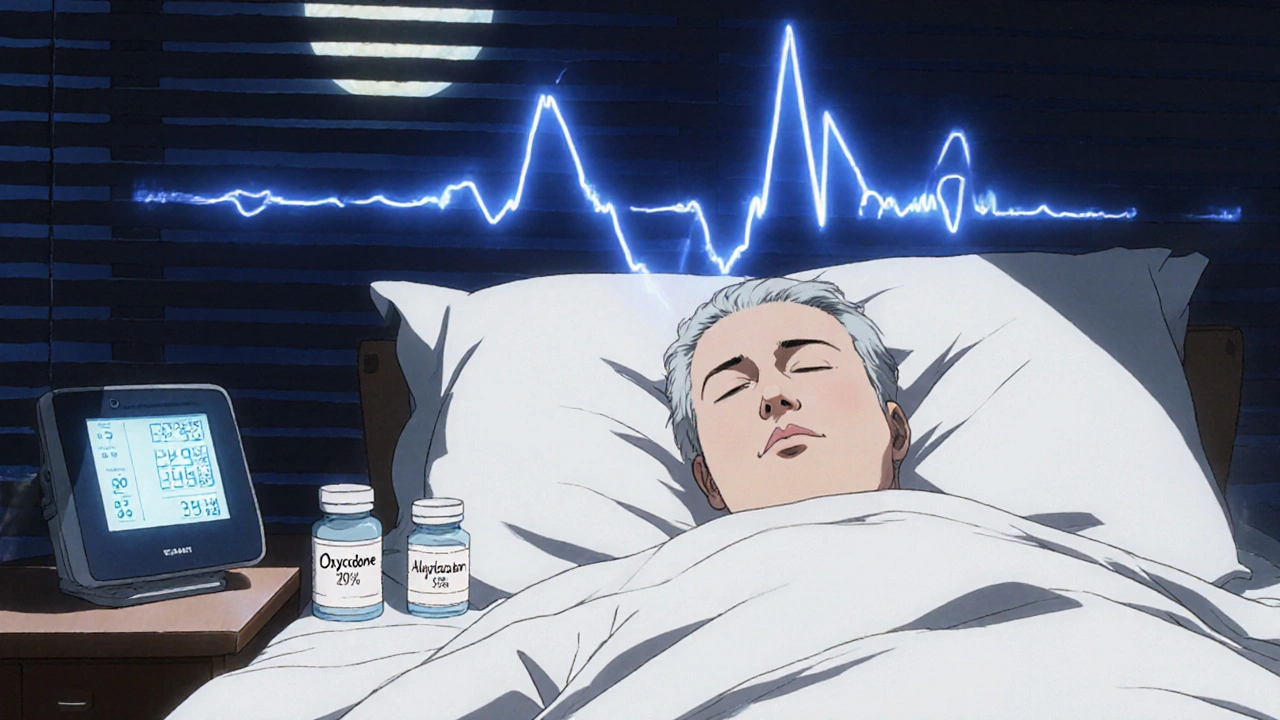
When you take opioids, a class of pain-relieving drugs that act on the brain’s reward and pain centers. Also known as narcotics, they include medications like oxycodone, hydrocodone, and morphine. And when you add benzodiazepines, a group of sedatives used for anxiety, insomnia, and muscle spasms. Also known as benzos, they include drugs like alprazolam, diazepam, and lorazepam. You’re not just doubling down on side effects—you’re stacking two drugs that slow your breathing. The FDA and CDC have warned that this combination is one of the most dangerous in modern medicine. It doesn’t just increase drowsiness. It can stop your breathing entirely, especially at night or when mixed with alcohol.
This isn’t theoretical. Thousands of overdose deaths each year involve both opioids and benzodiazepines. Even if you’re taking them as prescribed, the risk doesn’t disappear. Your body doesn’t build tolerance evenly—your brain’s ability to trigger a breathing reflex gets dulled faster than you realize. Doctors now avoid prescribing both at the same time unless there’s no other option, and even then, they monitor closely. If you’re on one of these, ask if you really need the other. Many people find relief with non-addictive alternatives: physical therapy for pain, CBT for anxiety, or sleep hygiene for insomnia. The goal isn’t to scare you—it’s to make sure you’re not stuck with a combination that could kill you without you knowing it.
What you’ll find in the posts below isn’t just a list of warnings. It’s a practical guide to understanding how these drugs work, how they interact with other medications like statins or antidepressants, and what real alternatives exist. You’ll see how REMS programs track high-risk prescriptions, how boxed warnings are changing, and why some drug combinations are banned while others are quietly phased out. This isn’t about fear—it’s about control. Knowing the risks lets you ask better questions, push back when needed, and choose safer paths. The information here isn’t just for patients—it’s for anyone who cares about someone who’s on these drugs. Because sometimes, the most powerful thing you can do is ask: Is this really necessary?