SSRIs and Opioids: Risks, Interactions, and What You Need to Know
When you take SSRIs, selective serotonin reuptake inhibitors used to treat depression and anxiety. Also known as antidepressants, they work by increasing serotonin in the brain to improve mood. Many people also take opioids, pain relievers like oxycodone, hydrocodone, or tramadol that act on the nervous system. Also known as narcotics, they’re prescribed for moderate to severe pain. The problem? These two types of drugs don’t just coexist—they can clash in ways that put your life at risk.
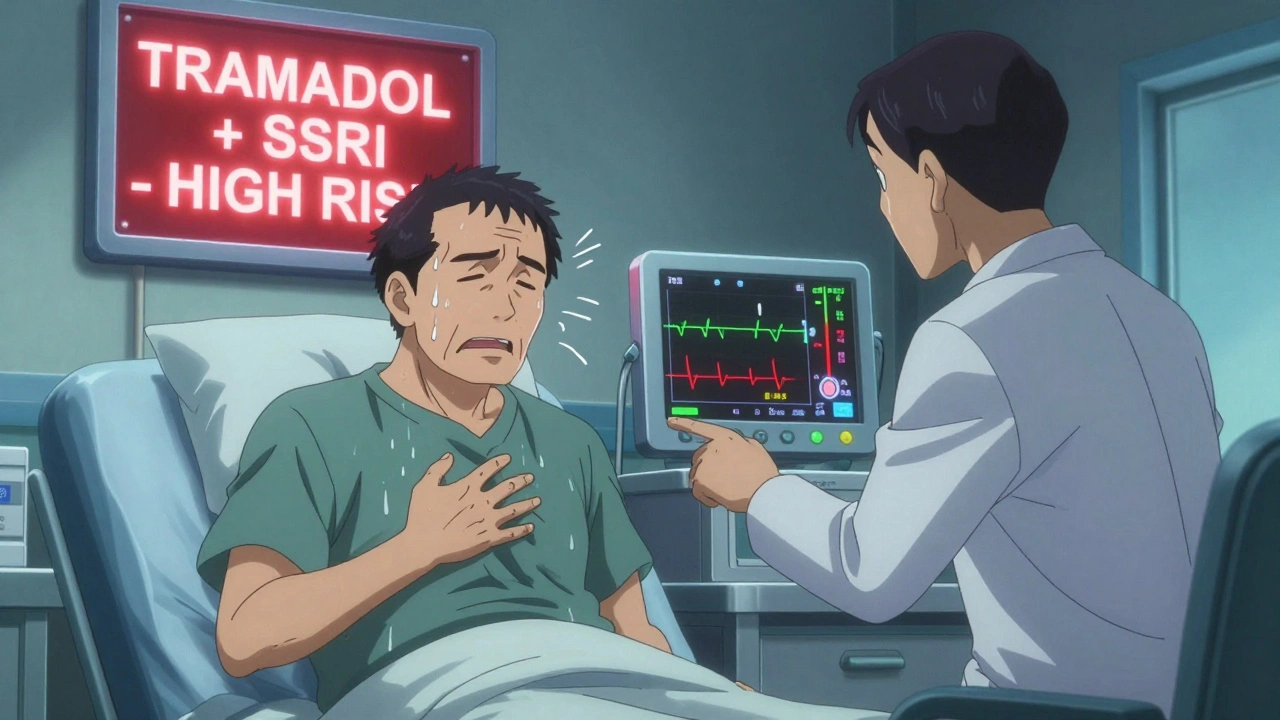
When SSRIs and opioids mix, your body can flood with too much serotonin. That’s not a theory—it’s a documented danger. serotonin syndrome, a potentially fatal reaction caused by excess serotonin in the nervous system shows up as confusion, rapid heart rate, high blood pressure, muscle rigidity, and sometimes seizures. It doesn’t always come from illegal drugs. It can start with a simple prescription change: your doctor adds tramadol for back pain while you’re already on sertraline for anxiety. No warning. No check-in. Just two common meds, doing damage you didn’t see coming.
Tramadol is especially risky because it doesn’t just act like an opioid—it also blocks serotonin reuptake, doubling down on the effect of SSRIs. Even codeine or morphine can be dangerous when paired with fluoxetine or escitalopram. And it’s not just about the drugs themselves. Age, liver function, kidney health, and other medications you’re taking can make the risk worse. Older adults on multiple prescriptions are the most vulnerable, but it can happen to anyone. You might not feel anything at first. Then, suddenly, you’re sweating, shaking, and struggling to breathe.
Some people think if it’s prescribed, it’s safe. That’s not true. The FDA has warned about this combination for years. The CDC says over 15% of opioid-related deaths involve antidepressants. But most patients never hear this from their doctor. Pharmacists flag it sometimes—but only if they catch it. You need to ask. You need to know. If you’re on an SSRI and your pain doctor adds a new opioid, pause. Ask: Could this cause serotonin syndrome? Is there a safer painkiller? Could we try physical therapy, NSAIDs, or a different approach?
This isn’t about avoiding medication. It’s about using it wisely. Many people need both SSRIs and opioids at different times in their lives. The goal isn’t to scare you—it’s to empower you. The posts below show you how to read your own drug labels, spot hidden interactions, and talk to your healthcare team with confidence. You’ll find real stories about people who missed the warning signs, and others who caught them in time. You’ll see how the FDA tracks these reactions, how generics can still carry the same risks, and why even over-the-counter cough medicines can make things worse.
Don’t assume your doctor knows every interaction. Don’t assume your pharmacist caught it. And don’t wait until you feel something strange to act. Knowledge isn’t just helpful here—it’s lifesaving.