Diabetes and Obesity: How Medications, Risks, and Lifestyle Intersect
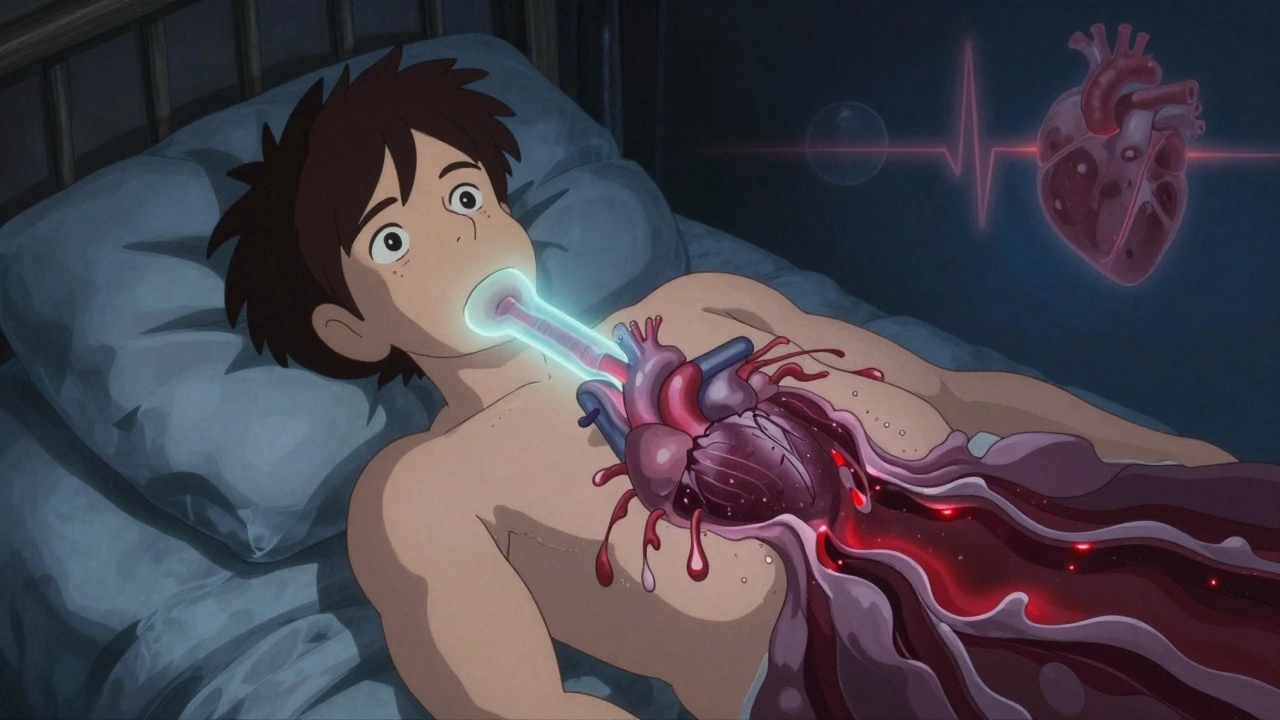
When you're dealing with diabetes and obesity, a pair of interconnected metabolic conditions that drive chronic illness and complicate medication use. Also known as metabolic syndrome, it's not just about weight or blood sugar—it's about how drugs, diet, and body chemistry collide in dangerous ways. Over 460 million people worldwide have diabetes, and nearly 90% of those with type 2 also live with obesity. The two don’t just coexist—they feed each other. Excess fat, especially around the belly, makes your cells resistant to insulin, forcing your pancreas to pump out more. Over time, it burns out. That’s when medications become necessary—and risky.
Many of the drugs used to treat diabetes and obesity interact with other common medications in ways most patients never see coming. Take SSRIs, a class of antidepressants often prescribed to people with diabetes who also struggle with depression. When mixed with certain painkillers like tramadol, they can trigger serotonin syndrome—a rare but deadly reaction. Or consider rifampin, a tuberculosis drug that speeds up how fast your liver breaks down other medications. If you’re on insulin or oral diabetes meds, rifampin can drop your blood sugar dangerously low without warning. Even something as simple as grapefruit can interfere with statins, which many people with obesity and diabetes take to protect their hearts. These aren’t edge cases. They’re everyday risks.
It’s not just about pills. Skipping doses, mixing OTC meds like dextromethorphan with antidepressants, or ignoring diet changes can turn manageable conditions into emergencies. The FDA’s REMS programs, safety systems designed for high-risk medications, exist because these interactions kill. And when patients don’t take their meds as prescribed—often because they’re overwhelmed or can’t afford them—the result is more hospital visits, more complications, and more deaths. The real problem isn’t the drugs. It’s the lack of clear, practical guidance on how they work together in real life.
What you’ll find below isn’t theory. It’s what people actually face: how to read drug labels to spot hidden dangers, why combination pills help adherence, how to avoid counterfeit meds, and what to ask your doctor before adding a new drug to your stack. These aren’t abstract concerns. They’re daily decisions that keep you alive—or put you in the ER.