Geriatric Medication Safety: Protecting Seniors from Dangerous Drug Interactions
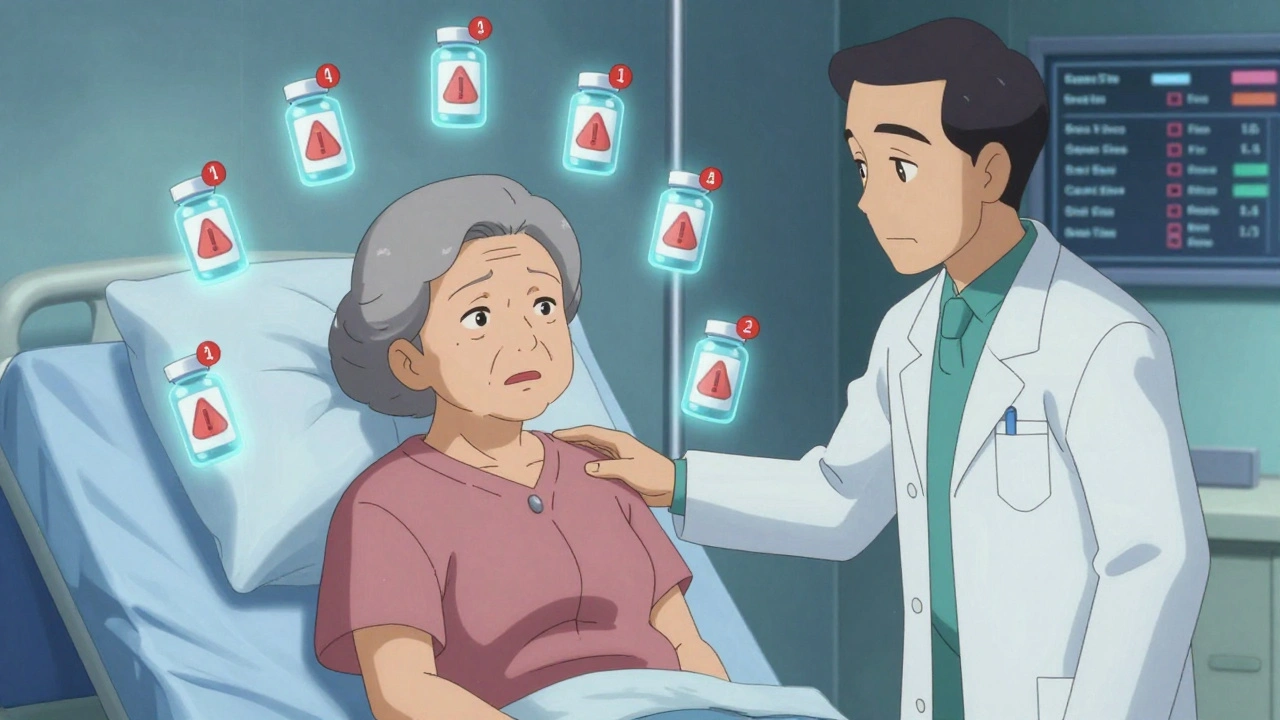
When it comes to geriatric medication safety, the practice of managing drug use in older adults to prevent harm from side effects, interactions, and improper dosing. Also known as safe prescribing for seniors, it’s not just about giving the right pill—it’s about knowing which pills shouldn’t be given together. About 40% of adults over 65 take five or more medications daily. That’s not just common—it’s a ticking time bomb. Each new drug adds risk, and the body changes with age. Liver and kidney function slow down. The brain gets more sensitive. What was safe at 50 can turn deadly at 75.
One of the biggest threats is polypharmacy, the use of multiple medications at once, often without clear purpose or coordination. Also known as drug burden, it’s not always the doctor’s fault. Patients might get prescriptions from different specialists, fill pills at different pharmacies, and forget what they’re even taking. This is why medication nonadherence, when patients skip, double up, or stop pills without telling anyone. Also known as pill skipping, is so common in older adults—it’s not laziness, it’s confusion. A senior might stop their blood pressure pill because they feel dizzy, not realizing the dizziness came from mixing it with a new painkiller. Or they take an over-the-counter cough syrup with MAOIs and trigger serotonin syndrome. These aren’t rare mistakes. They’re preventable tragedies.
The FDA drug safety, the system of oversight that monitors drugs after they reach the market, including adverse event reporting and import inspections. Also known as post-market surveillance, tries to catch these problems—but it can’t catch everything. That’s why families and caregivers need to be the first line of defense. Ask: Is this drug still needed? Could it interact with another? Is there a safer alternative? Check for black box warnings. Read the small print on the label. Talk to the pharmacist, not just the doctor. The FDA’s FAERS database shows thousands of cases where seniors ended up in the ER because of drug clashes. Many of those cases involved common meds: statins, antidepressants, painkillers, and sleep aids.
There’s no magic bullet, but there are clear steps. Simplify the regimen. Use one pharmacy. Keep a written list of every pill, including supplements. Watch for new symptoms—dizziness, confusion, falls, nausea—that might not seem drug-related but are. And never assume a pill is safe just because it’s over-the-counter. Dextromethorphan in cough syrup, antihistamines in sleep aids, even herbal supplements like St. John’s Wort—they all carry hidden risks for seniors. The goal isn’t to stop treatment. It’s to make every dose count, and every pill safe.
Below, you’ll find real-world guides that show exactly how these risks play out—and how to stop them before they start. From spotting dangerous combinations to reading drug labels like a pro, these posts give you the tools to protect someone you love.